When your child tugs at their ear, cries more than usual, or won’t sleep through the night, it’s easy to jump to one conclusion: an ear infection. And you’re not wrong. Acute otitis media (AOM) is the most common reason kids see a doctor in the U.S., with over 5 million cases every year. But here’s what most parents don’t know - ear infections don’t always need antibiotics. In fact, many clear up on their own. The real challenge isn’t just recognizing the infection - it’s knowing when to wait, when to treat, and when to consider tubes.
What Exactly Is an Ear Infection?
An ear infection isn’t just a sore ear. It’s a bacterial or viral infection in the middle ear - the space behind the eardrum. For a true diagnosis, three things must be present: sudden onset of symptoms, fluid trapped behind the eardrum (seen as a bulging or stiff eardrum), and signs of inflammation like redness or pain. It’s not just about fussiness. Severe cases mean a fever over 102.2°F, constant crying for hours, or pain that lasts more than 48 hours. Kids between 6 and 24 months are most at risk, and by age 3, about 83% of children have had at least one.When Antibiotics Are Necessary
Antibiotics aren’t the first step for every ear infection. But they’re critical in specific cases. If your child is under 6 months old, antibiotics are almost always needed - their immune systems aren’t strong enough to fight off the infection alone. Same goes for kids with severe symptoms: high fever, intense ear pain, or fluid draining from the ear. If the infection is in both ears and your child is between 6 and 23 months, antibiotics are strongly recommended too. The go-to antibiotic is high-dose amoxicillin - 80 to 90 milligrams per kilogram of body weight per day. For most kids, that’s a 10-day course. If your child has a penicillin allergy, alternatives like cefdinir, ceftriaxone, or clindamycin are used. But here’s the catch: antibiotics don’t work instantly. Pain relief comes first. Studies show nearly 7 out of 10 kids with ear infections have significant pain, yet less than 4 in 10 get proper pain meds. Acetaminophen or ibuprofen - given regularly - do more to help than most parents realize.Watchful Waiting: The Smart Alternative
You might be surprised to learn that 60 to 80% of ear infections get better without antibiotics. That’s why watchful waiting - also called delayed prescribing - is now a standard recommendation. It means holding off on antibiotics for 48 to 72 hours while monitoring symptoms closely. This approach works best for kids over 2 years old with mild symptoms, whether the infection is in one ear or both. Even for kids between 6 and 23 months, if it’s only one ear and symptoms aren’t severe, waiting is safe. During watchful waiting, you’re not just waiting around. You’re actively watching. If the pain doesn’t improve after two days, if the fever spikes, or if your child seems worse, that’s when you call the doctor for a prescription. In fact, 67% of parents who use this method end up filling an antibiotic prescription anyway - but only because they needed it, not because it was given upfront. The CDC reports that only about one-third of children in watchful waiting programs actually end up needing antibiotics. And here’s the best part: research shows no increase in complications like hearing loss or ruptured eardrums when this approach is followed correctly.
Tympanostomy Tubes: For Recurrent or Persistent Cases
If your child keeps getting ear infections - three in six months or four in a year - tubes might be the next step. These tiny plastic tubes are inserted through the eardrum during a quick outpatient procedure. Their job? To let air into the middle ear and drain fluid that keeps building up. Tubes stay in place for 6 to 18 months before falling out on their own. Tubes aren’t for every child who gets an occasional ear infection. They’re recommended only when infections are frequent and there’s lasting fluid behind the eardrum causing hearing loss - usually 40 decibels or more. That’s the kind of hearing loss that can delay speech development. About 667,000 tube surgeries are done each year in the U.S., costing billions. But they work: in the first six months after insertion, kids have about half as many infections. After that, the benefit fades. Some experts warn tubes are overused in kids who just have frequent infections but no hearing problems.What Doesn’t Work - And Why
You’ve probably heard advice like giving your child decongestants, antihistamines, or nasal sprays for ear infections. Don’t. Multiple studies show these don’t help. In fact, they can cause side effects like drowsiness, irritability, or even faster heart rates in young kids. The CDC says the number needed to treat (NNT) for any benefit is 20 - meaning you’d have to give it to 20 kids to help one, and 15% of them would have bad reactions. Same goes for home remedies like garlic oil or warm compresses. They might soothe discomfort, but they don’t treat the infection.Why Do So Many Kids Still Get Antibiotics?
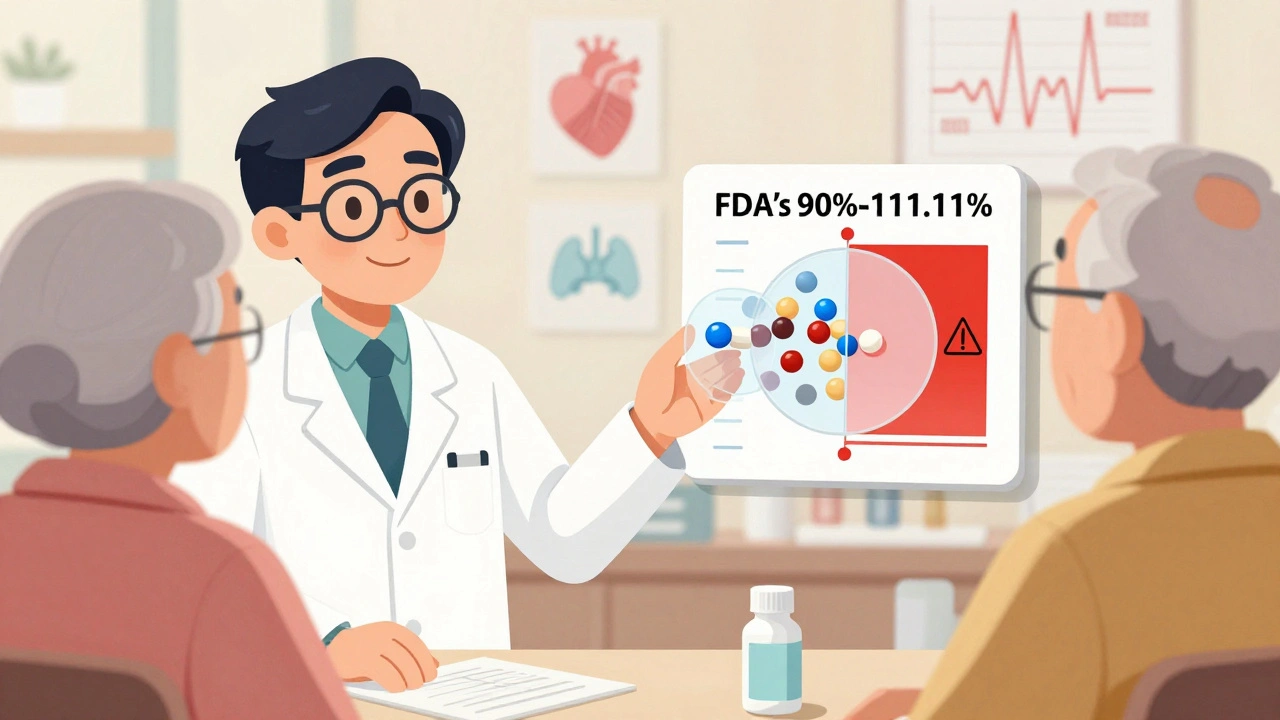
If the guidelines are clear, why do so many doctors still prescribe antibiotics right away? Because it’s easier. Parents are anxious. They want something done. Doctors are pressed for time. In one study, 41% of clinicians said parental pressure led them to prescribe antibiotics even when they didn’t think they were needed. Another 68% cited time constraints - explaining watchful waiting takes longer than handing out a script. And 33% admit they’re unsure about the diagnosis, especially when the eardrum looks unclear. But things are changing. Hospitals that use automated prompts in their electronic records cut inappropriate prescribing by 29%. Clinics that give parents safety-net prescriptions - a paper or digital script they can fill only if symptoms worsen - saw 76% compliance. Decision aids, like simple charts showing when to wait and when to act, increased proper antibiotic use by 22%. The bottom line: when parents are educated, they’re more likely to choose the right path.
What’s Changing in the Guidelines
The latest guidelines, updated in 2013, already made big shifts. Before that, antibiotics were routinely given to all kids under 2. Now, for a healthy 18-month-old with a single ear infection and mild symptoms, waiting is fine. The 2024 revision, still in draft, will tighten tube criteria even more - requiring documented hearing loss before surgery for all kids. It will also expand watchful waiting to include some bilateral cases in children over 2. Vaccines are helping too. Since the introduction of the pneumococcal conjugate vaccine (PCV13) in 2010, ear infection rates have dropped by 12%, and recurrent cases by 20%. That’s millions fewer infections. The CDC reports antibiotic prescribing for ear infections has fallen from 95% in 1995 to just 61% in 2022. We’re getting closer to the Healthy People 2030 goal of 50%.What You Can Do Right Now
If your child has an ear infection:- Give acetaminophen or ibuprofen regularly - don’t wait for the pain to get worse.
- Watch for signs of improvement in 48 hours. If they’re not better, or if they’re worse, call your doctor.
- Ask: ‘Is this severe? Is it in both ears? Is my child under 2?’ That helps you understand if antibiotics are truly needed.
- If your doctor suggests watchful waiting, ask for a safety-net prescription. Keep it on hand, but don’t fill it unless symptoms don’t improve.
- If infections keep coming back, ask about hearing tests. Persistent fluid and hearing loss are the real reasons tubes are recommended.
Final Thought: Less Is More
It’s hard to watch your child in pain. You want to fix it fast. But sometimes, the most powerful thing you can do is wait - and comfort. Antibiotics save lives, but they’re not magic bullets. Overuse fuels antibiotic resistance, which already causes 2.8 million infections and 35,000 deaths in the U.S. every year. Tubes can help, but they’re not a quick fix for every ear infection. The best care isn’t about doing more. It’s about doing the right thing at the right time.Do all ear infections need antibiotics?
No. About 60 to 80% of ear infections in children clear up on their own within a few days. Antibiotics are only needed for severe cases, infants under 6 months, or infections in both ears for children 6 to 23 months old. For mild cases in older kids, watchful waiting is safe and recommended.
How do I know if my child’s ear infection is severe?
Signs of a severe ear infection include a fever over 102.2°F (39°C), ear pain lasting more than 48 hours, constant crying, trouble sleeping, or fluid draining from the ear. If your child appears very sick or is unusually lethargic, seek care immediately. Mild cases involve fussiness, mild ear tugging, and low-grade fever without these red flags.
What is watchful waiting, and is it safe?
Watchful waiting means delaying antibiotics for 48 to 72 hours while giving pain relief and watching for improvement. It’s safe for children over 2 with mild symptoms and for those 6 to 23 months with a single ear infection and no severe signs. Studies show only about one-third of these kids end up needing antibiotics, and there’s no increase in complications like hearing loss or ruptured eardrums.
When are ear tubes recommended?
Tubes are recommended if a child has three ear infections in six months or four in a year, with at least one in the last six months - and if there’s persistent fluid behind the eardrum causing hearing loss of 40 decibels or more. They’re not for occasional infections. The goal is to prevent hearing delays, not just reduce infection frequency.
Can ear infections cause hearing loss?
Yes, but usually temporary. Fluid trapped behind the eardrum can block sound, causing mild to moderate hearing loss - often around 20 to 40 decibels. This can affect speech development if it lasts for months. If hearing loss lasts longer than three months, a hearing test is needed. Permanent hearing loss from ear infections is rare.
Are decongestants or antihistamines helpful?
No. Studies show these medications don’t help with ear infections. In fact, they can cause side effects like drowsiness, irritability, or increased heart rate in young children. The CDC and major pediatric guidelines strongly advise against using them for ear infections.
How can I prevent ear infections in my child?
Vaccines like PCV13 (pneumococcal conjugate) reduce ear infections by 12% and recurrent ones by 20%. Avoid exposing your child to secondhand smoke, breastfeed if possible, and limit pacifier use after 6 months. Bottle-feeding while lying down increases risk, so feed upright. Regular handwashing also helps reduce colds, which often lead to ear infections.







15 Comments