Benzodiazepine-Opioid Risk Calculator
This tool demonstrates how the combination of opioids and benzodiazepines increases the risk of respiratory depression and overdose. When taken together, these medications don't just add risk—they multiply it.
According to CDC data: People prescribed both opioids and benzodiazepines are 10 times more likely to die from an opioid overdose than those taking opioids alone.
Note: This calculator illustrates the risk increase based on available medical data. It is not a substitute for professional medical advice.
Important Note: This tool demonstrates the dangerous synergy between these medications. Even at therapeutic doses, the combination can lead to fatal respiratory depression. Always consult with a healthcare professional before taking any medications.
When you take an opioid for pain and a benzodiazepine for anxiety, you might think you’re managing two separate problems. But what you’re really doing is putting your breathing at risk-potentially fatally. The combination of these two drug classes doesn’t just add up; it multiplies danger. In 2019, nearly 1 in 6 opioid overdose deaths in the U.S. involved benzodiazepines. That’s not a coincidence. It’s a deadly synergy.
How Opioids Slow Your Breathing
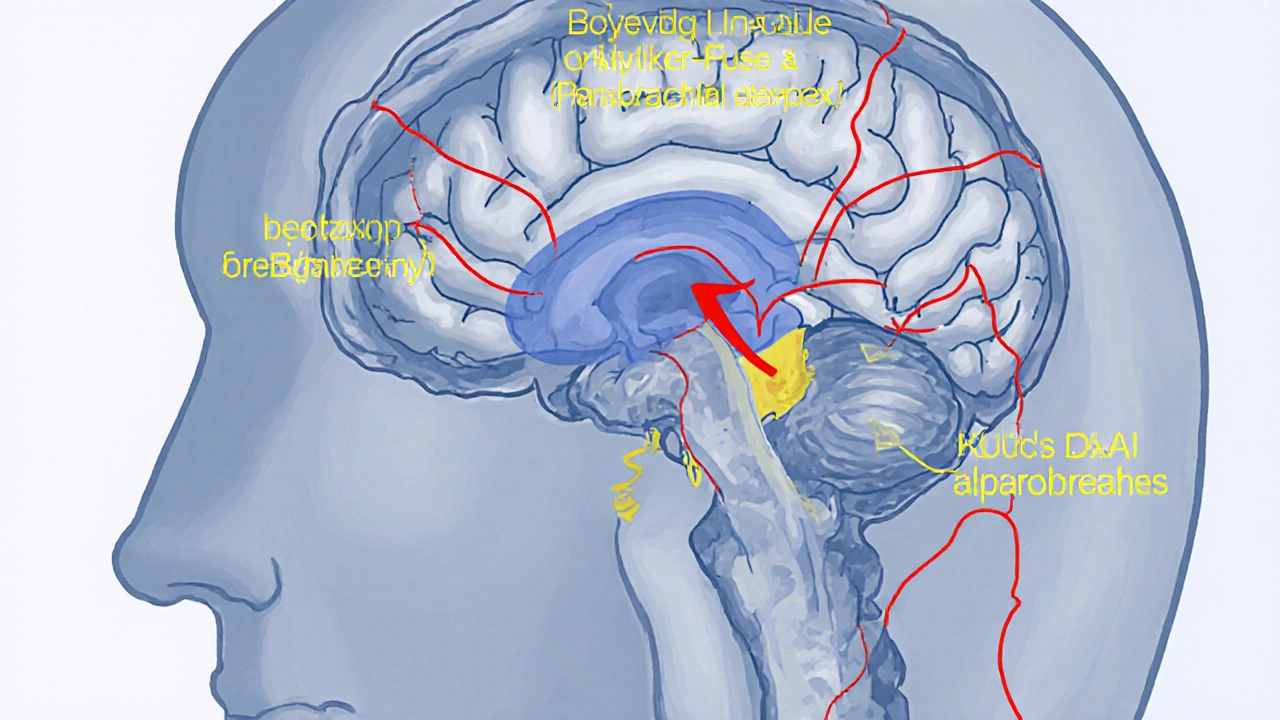
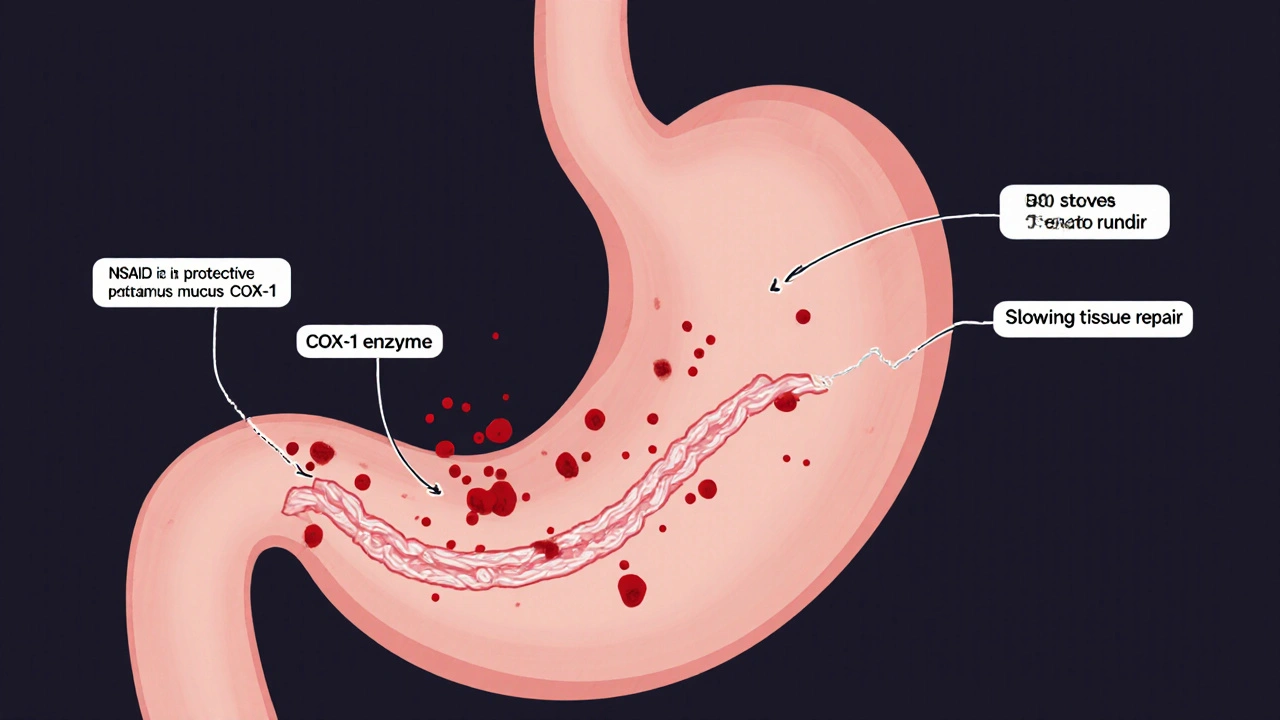
Opioids like oxycodone, hydrocodone, fentanyl, and heroin work by binding to mu-opioid receptors in the brainstem. These receptors control the automatic rhythm of breathing. When activated, they don’t just dull pain-they quiet the brain’s drive to inhale and exhale. Studies show opioids stretch out the exhale phase, causing longer pauses between breaths. This isn’t just drowsiness. It’s a suppression of the body’s most basic survival function. The Kölliker-Fuse/Parabrachial complex (KF/PB) in the brainstem is one key area affected. Opioids here increase expiratory drive, making each exhale last too long. Meanwhile, the preBötzinger Complex-the brain’s main rhythm generator for breathing-gets suppressed. Neurons there become less active, reducing the number of breaths per minute. Even at therapeutic doses, opioids can slow breathing. At higher doses, they can stop it entirely.How Benzodiazepines Make It Worse
Benzodiazepines like diazepam, alprazolam, and lorazepam work differently. They boost GABA, the brain’s main calming chemical. This reduces nerve activity across the central nervous system, including the areas that control breathing. Alone, benzodiazepines rarely cause serious respiratory depression in healthy people. But when paired with opioids, the effect isn’t just additive-it’s explosive. A 2018 study found that when fentanyl and midazolam were given together, minute ventilation dropped by 78%. Fentanyl alone caused a 45% drop. Midazolam alone? Just 28%. That’s not 73% added together. It’s 78%. The combination creates a double hit: opioids silence the brain’s breathing command center, and benzodiazepines mute the backup systems that might kick in to compensate. This synergy hits hardest in the brainstem regions that manage the transition between inhaling and exhaling. The result? Shallow, irregular breathing. Long pauses. Then, silence.The Numbers Don’t Lie
The CDC reports that people prescribed both opioids and benzodiazepines are 10 times more likely to die from an opioid overdose than those taking opioids alone. Between 2010 and 2021, opioid overdose deaths jumped from 21,089 to over 80,000. More than three-quarters of those deaths involved other drugs-most often benzodiazepines or alcohol. The highest risk group? People aged 45 to 64. In 2020, this group saw 22.3 deaths per 100,000 from combined opioid and benzodiazepine use. That’s more than double the rate for younger adults. Many of these individuals were prescribed both drugs for chronic pain and anxiety-often by different doctors, without coordination. Between 2004 and 2011, emergency room visits from nonmedical use of both drugs rose by 131%. In 2019, the fatality rate from this combination had climbed 1,800% since 1999. These aren’t abstract trends. These are real people-parents, coworkers, neighbors-whose breathing stopped because two legal prescriptions interacted in ways their doctors didn’t fully warn them about.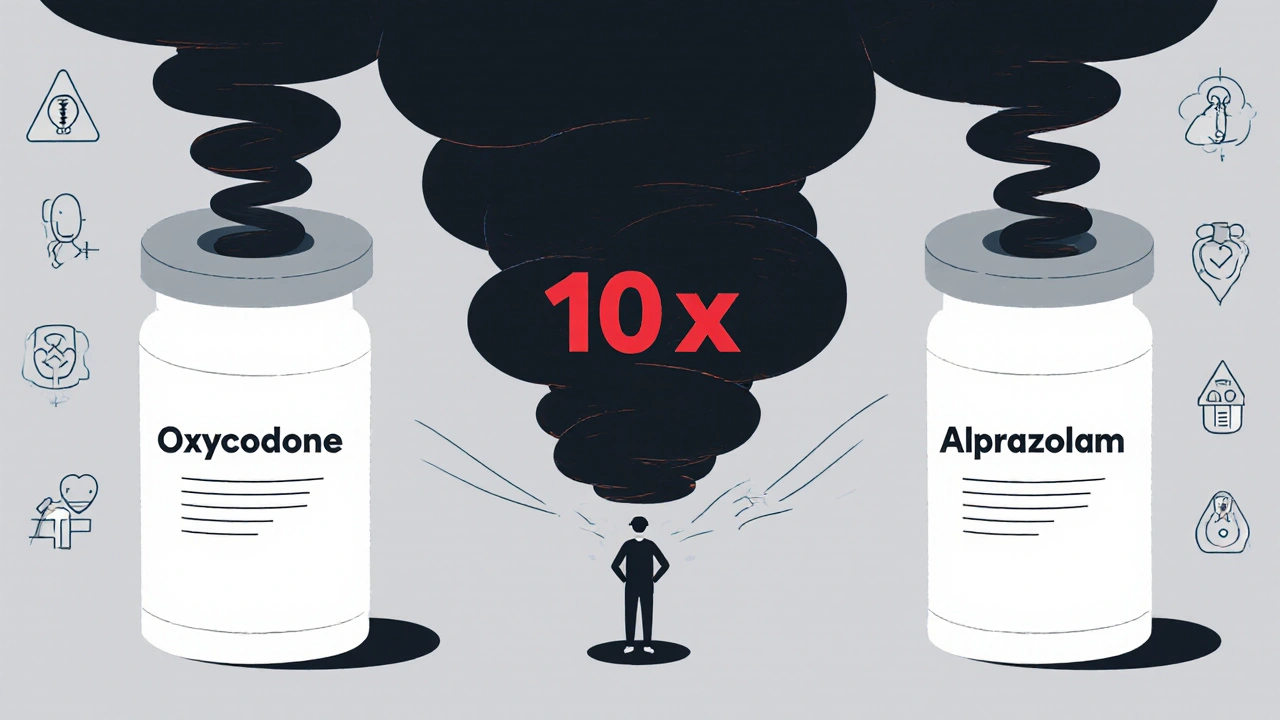
Why Doctors Still Prescribe Both
Despite clear warnings from the FDA, CDC, and American Society of Anesthesiologists, the practice hasn’t disappeared. In 2022, 8.7% of patients on long-term opioid therapy were still getting benzodiazepines at the same time. Some doctors believe benzodiazepines help with muscle spasms or severe anxiety that doesn’t respond to other treatments. Others simply don’t realize how dangerous the combo is. The FDA issued a black box warning in 2016-the strongest possible alert-stating that combining these drugs can lead to profound sedation, coma, or death. Yet prescribing patterns changed only slightly. After the warning, concurrent prescribing dropped by 14.5%. That’s progress. But it’s not enough. The problem is compounded when patients see multiple providers. One prescribes oxycodone for back pain. Another prescribes alprazolam for panic attacks. Neither knows the other’s prescription. Pharmacies don’t always flag the risk. Patients don’t always tell their doctors everything they’re taking.What Can Be Done Instead
There are safer alternatives for both pain and anxiety. For anxiety, SSRIs like sertraline or escitalopram are first-line treatments. They don’t suppress breathing. Buspirone is another non-addictive option for generalized anxiety. For chronic pain, non-opioid options like physical therapy, cognitive behavioral therapy, acetaminophen, or NSAIDs (when appropriate) should be tried first. For patients who truly need both medications-say, someone with severe PTSD and chronic pain-the guidelines are clear: use the lowest possible doses for the shortest possible time. Monitor closely. Avoid long-acting formulations. Never combine with alcohol or sleeping pills. And always have naloxone on hand.Naloxone Isn’t Enough
Naloxone can reverse opioid overdose. It’s life-saving. But it does nothing for benzodiazepine-induced respiratory depression. If someone overdoses on both drugs, naloxone might wake them up-but their breathing can still stop because the benzodiazepine is still active in their system. That’s why some researchers are working on new reversal agents. One experimental compound, CX1739, restored breathing in animal models exposed to fentanyl and alprazolam. But it’s not yet available to the public. Until then, naloxone is still critical-but it’s only half the solution.What You Need to Know
If you’re taking an opioid for pain:- Ask your doctor: Is a benzodiazepine really necessary?
- If you’re already taking one, don’t stop suddenly. Talk to your provider about tapering safely.
- Never mix these drugs with alcohol, sleeping pills, or street drugs.
- Keep naloxone at home. Know how to use it. Teach someone else how to use it too.
- Be honest with your doctor about any pain medications you’re using.
- Ask if there’s a non-sedating alternative.
- Watch for signs of slowed breathing: confusion, dizziness, blue lips, or difficulty staying awake.





10 Comments