Capecitabine is an oral prodrug of 5‑fluorouracil (5‑FU) that converts to the active chemotherapy agent inside tumor cells. It was approved in 1998 and is now a cornerstone of adjuvant therapy for several solid tumours.
Why Preventing Recurrence Matters
After curative surgery, the biggest threat is microscopic disease that can spring back months or years later. Studies consistently show that patients who receive effective adjuvant treatment enjoy longer disease‑free survival (DFS) and lower overall mortality. In everyday practice, the decision to add a drug hinges on its ability to shave off even a few percentage points of recurrence risk without adding unbearable toxicity.
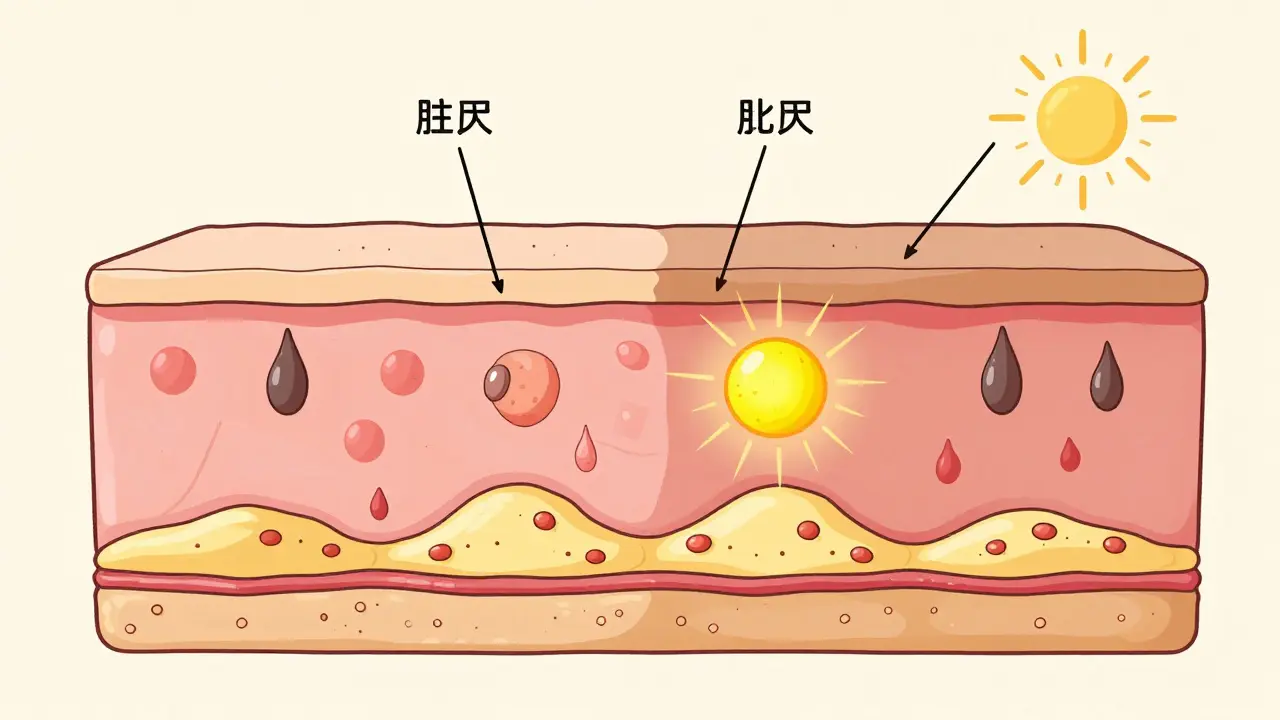
How Capecitabine Works Inside the Body
The magic happens through a three‑step enzymatic cascade. First, capecitabine is absorbed in the gut and converted to 5′‑deoxy‑5‑fluorocytidine (5′‑dFCR) by carboxylesterase in the liver. Next, cytidine deaminase transforms 5′‑dFCR into 5′‑deoxy‑5‑fluorouridine (5′‑dFUR). Finally, tumour‑high thymidine phosphorylase (TP) turns 5′‑dFUR into active 5‑FU right where it’s needed.
This tumour‑selective activation means higher intratumour concentrations of 5‑FU while keeping systemic exposure comparatively low. The result is a potent anti‑DNA synthesis effect with fewer dose‑limiting side effects than continuous intravenous 5‑FU.
Clinical Evidence for Recurrence Prevention
Large phase III trials have quantified capecitabine’s impact on recurrence:
- Colorectal cancer (CAPOX/ XELOX): The MOSAIC‑C trial showed 5‑year DFS of 78% with capecitabine plus oxaliplatin versus 70% with surgery alone.
- Breast cancer (adjuvant setting): A meta‑analysis of six trials reported a 3.5% absolute reduction in 5‑year recurrence when capecitabine was added to standard regimens.
- Gastric cancer: The ACTS‑GC study demonstrated a hazard ratio of 0.71 for recurrence with capecitabine‑based chemoradiation.
These numbers translate into a tangible capecitabine recurrence prevention benefit for patients who can tolerate oral chemotherapy.
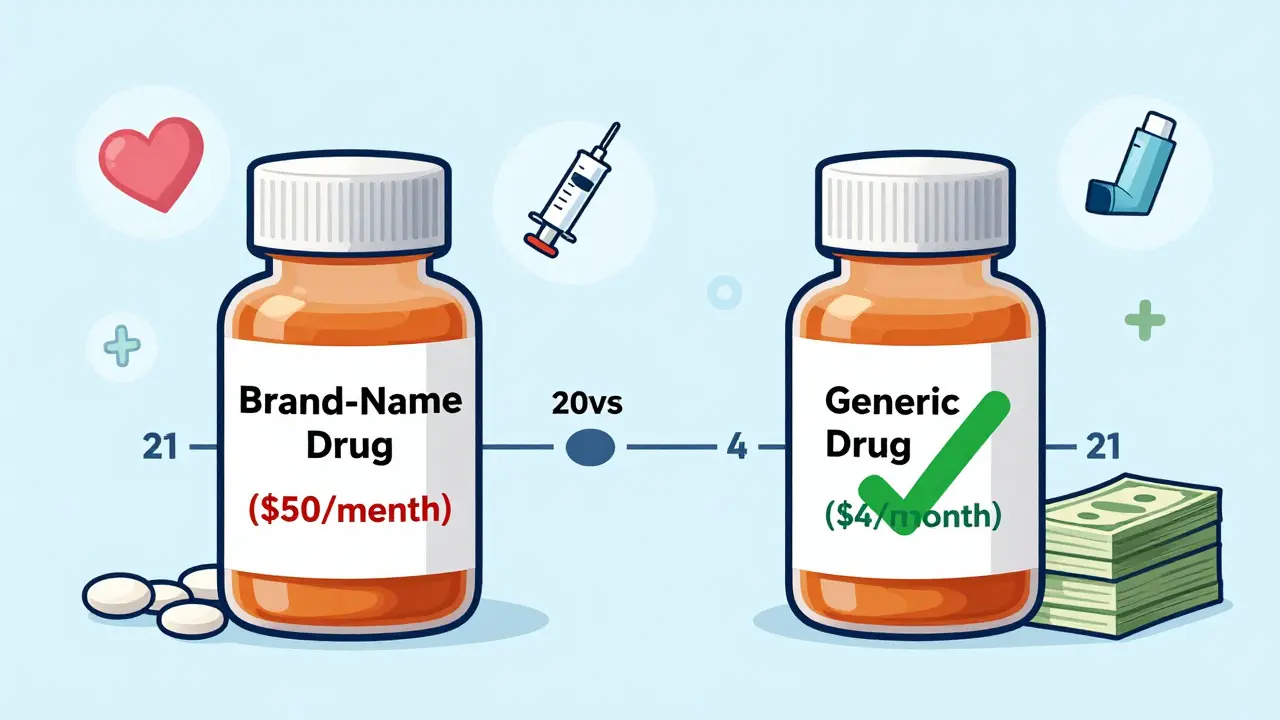
Comparing Capecitabine to Intravenous 5‑FU
Both drugs share the same active moiety, yet their delivery routes shape efficacy and patient experience. Below is a quick side‑by‑side look.
| Attribute | Capecitabine | IV 5‑FU |
|---|---|---|
| Administration | Oral, 2×daily for 14‑days cycles | Continuous infusion or bolus |
| Conversion Site | Tumour‑high thymidine phosphorylase | Systemic |
| Common Indications | Colorectal, breast, gastric, pancreatic | Colorectal, head‑neck, oesophageal |
| Recurrence Benefit | 5‑yr DFS ↑8‑10% | 5‑yr DFS ↑5‑7% |
| Typical Toxicities | Hand‑foot syndrome, diarrhea, nausea | Myelosuppression, mucositis |
Practical Considerations: Dosing, Side Effects, and Monitoring
Standard dosing for capecitabine in the adjuvant setting is 1,250mg/m² twice daily for 14 days followed by a 7‑day rest (one 3‑week cycle). Dose reductions of 25% are recommended for moderate renal impairment (creatinine clearance 30‑50ml/min) and for patients who develop grade2 hand‑foot syndrome.
Key toxicities to watch:
- Hand‑foot syndrome - redness and swelling on palms/soles; management includes dose interruption and topical emollients.
- Diarrhea - hydrate, use loperamide early.
- Elevated liver enzymes - check baseline and every 2‑3 cycles.
Regular blood counts and renal function tests are essential. Many oncology centres schedule labs on day1 of each cycle, making the monitoring schedule easy to fit into standard appointments.

Integrating Capecitabine into Combination Regimens
When paired with oxaliplatin, the regimen is known as CAPOX (or XELOX). This combo gained traction after the NO16968 trial showed a 6‑year DFS of 73% versus 68% with surgery alone for stageIII colon cancer.
For breast cancer, capecitabine can be added after taxane‑based chemotherapy-often called the “sequential capecitabine” approach. The CREATE‑X study highlighted a 4‑year disease‑free survival gain of 5.6% in triple‑negative disease.
Choosing the right partner drug depends on tumour biology, patient comorbidities, and prior exposure to neurotoxic agents.
Who Benefits Most? Patient Selection and Biomarkers
Not every patient is a perfect fit. Factors that tip the scales toward capecitabine include:
- Preference for oral therapy (avoids central line and infusion visits).
- Good renal function (eGFR>60ml/min).
- High tumour expression of thymidine phosphorylase - some labs offer TP immunohistochemistry, though it’s not yet standard of care.
- StageIII disease after curative resection, where adjuvant chemo is strongly indicated.
Emerging pharmacogenomic markers, such as DPYD variants, predict severe fluoropyrimidine toxicity. Testing for DPYD before initiating capecitabine can reduce hospitalisations by up to 30%.
Future Directions: New Formulations and Ongoing Trials
Researchers are exploring fixed‑dose combination tablets that merge capecitabine with targeted agents like bevacizumab. Early‑phase data suggest synergistic tumour suppression without adding extra hand‑foot toxicity.
Several phase III trials are underway:
- CAPEC-2: Capecitabine versus 5‑FU in stageII colon cancer after high‑risk pathological features.
- BREAST‑CAP: Adding capecitabine to HER2‑targeted therapy in early‑stage HER2‑positive disease.
These studies will clarify whether capecitabine can become the default oral partner for many adjuvant regimens.
Key Take‑aways
- Capecitabine’s tumour‑selective activation gives it a solid recurrence‑prevention edge over straight IV 5‑FU.
- Clinical trials consistently show 5‑10% absolute improvements in disease‑free survival.
- Oral dosing improves quality of life but requires diligent side‑effect monitoring.
- Combination regimens like CAPOX maximize benefit for stageIII colorectal cancer.
- Genetic testing (DPYD) and TP expression are emerging tools for personalising therapy.
Frequently Asked Questions
Can I take capecitabine at home or do I need a hospital infusion?
Capecitabine is an oral tablet, so you take it at home. The only hospital visits required are for blood work and periodic assessments. This makes it a convenient option for many patients who want to avoid a central line.
What are the most common side effects, and how can I manage them?
The top three are hand‑foot syndrome, diarrhea, and nausea. For hand‑foot, keep skin moisturised, avoid tight shoes, and report any redness early. Diarrhea is best handled with prompt loperamide and staying hydrated. Nausea often responds to mild anti‑emetics taken before each dose.
How does capecitabine compare to IV 5‑FU in preventing recurrence?
Both deliver the same active drug, but capecitabine’s tumor‑focused conversion yields slightly higher disease‑free survival rates (about 5‑10% absolute benefit) and offers the convenience of oral dosing. Intravenous 5‑FU may still be preferred when a patient cannot tolerate oral therapy or has severe renal impairment.
Is capecitabine safe for patients with mild kidney problems?
Mild renal impairment (eGFR>60ml/min) usually allows full dosing. If eGFR drops to 30‑50ml/min, a 25% dose reduction is recommended. Severe impairment (<30ml/min) is a contraindication.
Do I need genetic testing before starting capecitabine?
Testing for DPYD gene variants is increasingly advised because certain mutations raise the risk of life‑threatening toxicity. If a variant is found, the oncologist will adjust the dose or consider an alternative regimen.
Can capecitabine be combined with radiation therapy?
Yes. In gastrointestinal cancers, capecitabine‑based chemoradiation is a standard approach. The drug acts as a radiosensitiser, enhancing the effect of radiation on tumour cells while keeping systemic toxicity manageable.
What is the typical duration of adjuvant capecitabine treatment?
Most protocols prescribe six to eight cycles (about 4‑6months). Some studies extending treatment to 12months have not shown extra survival benefit and increase toxicity.





12 Comments