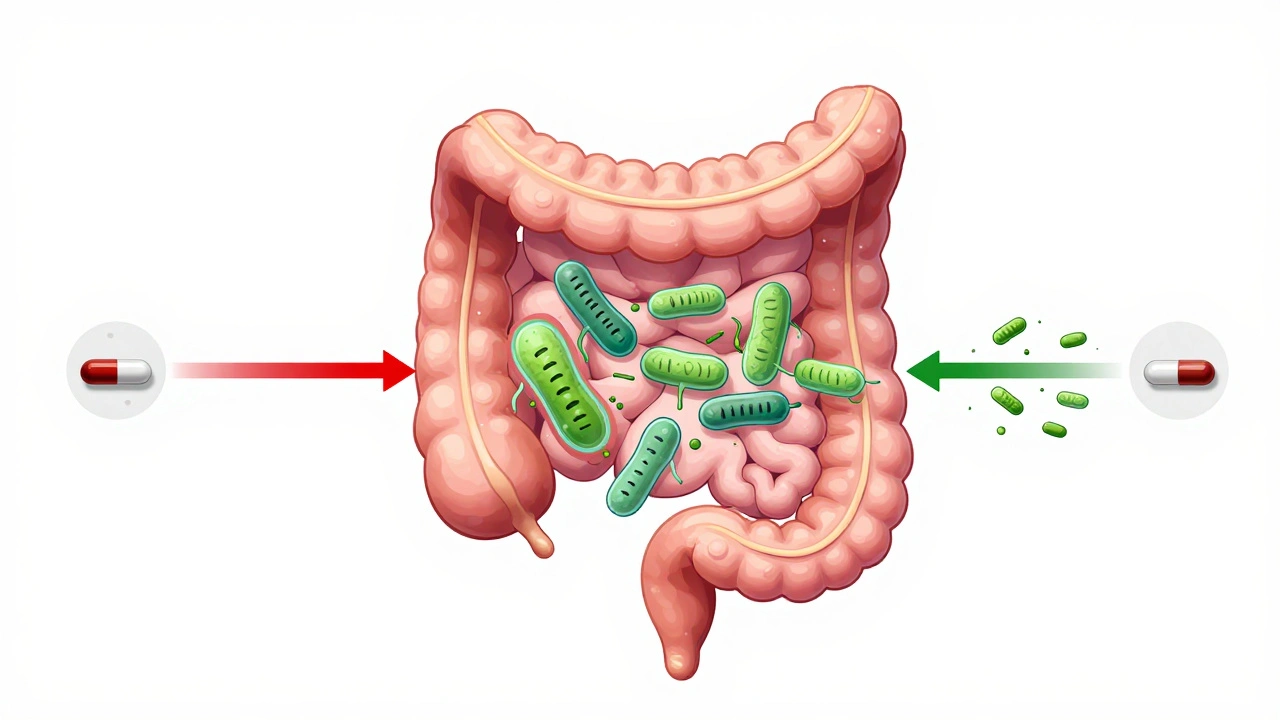
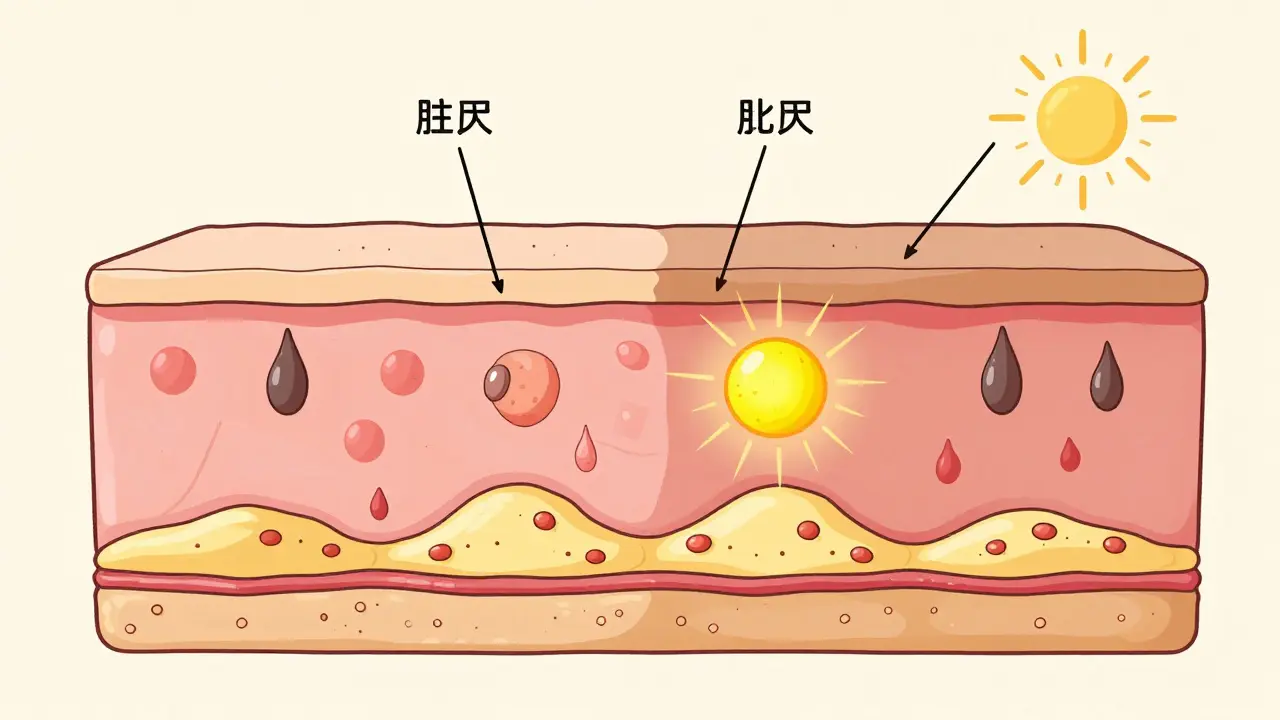
When you’re on antibiotics, your gut pays the price. Even if the medicine is doing its job killing bad bacteria, it’s also wiping out the good ones - the ones that keep your digestion smooth, your immune system sharp, and your energy steady. That’s why so many people end up with bloating, cramps, or diarrhea while taking antibiotics. But there’s a simple fix: taking probiotics at the right time. Not just any time. The spacing between your antibiotic and probiotic dose makes all the difference.
Why Timing Matters More Than You Think
Antibiotics don’t pick and choose. They hit everything in their path - harmful bacteria, yes, but also the helpful ones like Lactobacillus and Bifidobacterium. If you take a probiotic right after your antibiotic, those live cultures get wiped out before they even have a chance to settle in. Studies show that without proper spacing, up to 92% of the probiotic bacteria die off. That’s not just wasted money - it’s wasted protection. The goal isn’t just to survive the antibiotic course. It’s to come out of it with your gut still working. Research from the Journal of the American Medical Association and the International Scientific Association for Probiotics and Prebiotics (ISAPP) shows that when you space probiotics correctly, you cut your risk of antibiotic-associated diarrhea by more than half. That’s not a small win. One in three people on antibiotics get diarrhea. You don’t have to be one of them.The Two-Hour Rule: Simple, Proven, Effective
The gold standard is simple: take your probiotic at least two hours before or after your antibiotic dose. This isn’t a guess. It’s based on how long antibiotics stay active in your gut. Most antibiotics clear out of your digestive system within that window, giving your probiotics a safe chance to land and start working. For example, if you take amoxicillin at 8 a.m. and 8 p.m., your probiotic should go in at 6 a.m. and 6 p.m. - or even 10 a.m. and 10 p.m. The key is keeping that two-hour buffer. Some doctors even recommend four to six hours for stronger antibiotics like clindamycin or ciprofloxacin, especially if you’ve had gut issues before. Don’t think you can just take them together and hope for the best. In-vitro tests show that simultaneous dosing reduces probiotic survival by 78-92%. That’s not close enough. You need distance.Not All Probiotics Are the Same
Here’s where most people get confused. Not every probiotic needs the same treatment. There are two main types: bacterial and yeast. Bacterial strains - like Lactobacillus rhamnosus GG and Bifidobacterium lactis - are alive, just like the bacteria in your gut. And yes, antibiotics kill them. These need the two-hour gap. Then there’s Saccharomyces boulardii. This one’s a yeast, not a bacterium. Antibiotics don’t touch it. That means you can take it at the same time as your antibiotic. No waiting. No stress. And it’s one of the most effective strains for preventing diarrhea. Studies show it cuts AAD risk by 52% when taken at 20 billion CFUs per day. So check your label. If it says “yeast” or lists Saccharomyces boulardii, you’re in the clear. If it lists lactobacillus, bifidobacterium, or other bacteria, stick to the two-hour rule.How Much Should You Take?
Dose matters. Too little, and you won’t see results. Too much, and you might just get more gas. For most people on a short course (3-5 days), 5-10 billion CFUs a day is enough. That’s like a standard over-the-counter capsule. If you’ve had diarrhea before on antibiotics, or you’re on a longer course (7+ days), bump it up to 10-20 billion CFUs. For serious cases - like someone on 14+ days of antibiotics, or with a history of C. diff - go with 20-40 billion CFUs. That’s often a prescription-grade product. And here’s the kicker: multi-strain doesn’t mean better. A 2023 meta-analysis found no advantage to products with 10+ strains over single-strain ones. What matters is the strain itself and the dose. Stick with proven ones: L. rhamnosus GG and S. boulardii have the strongest data.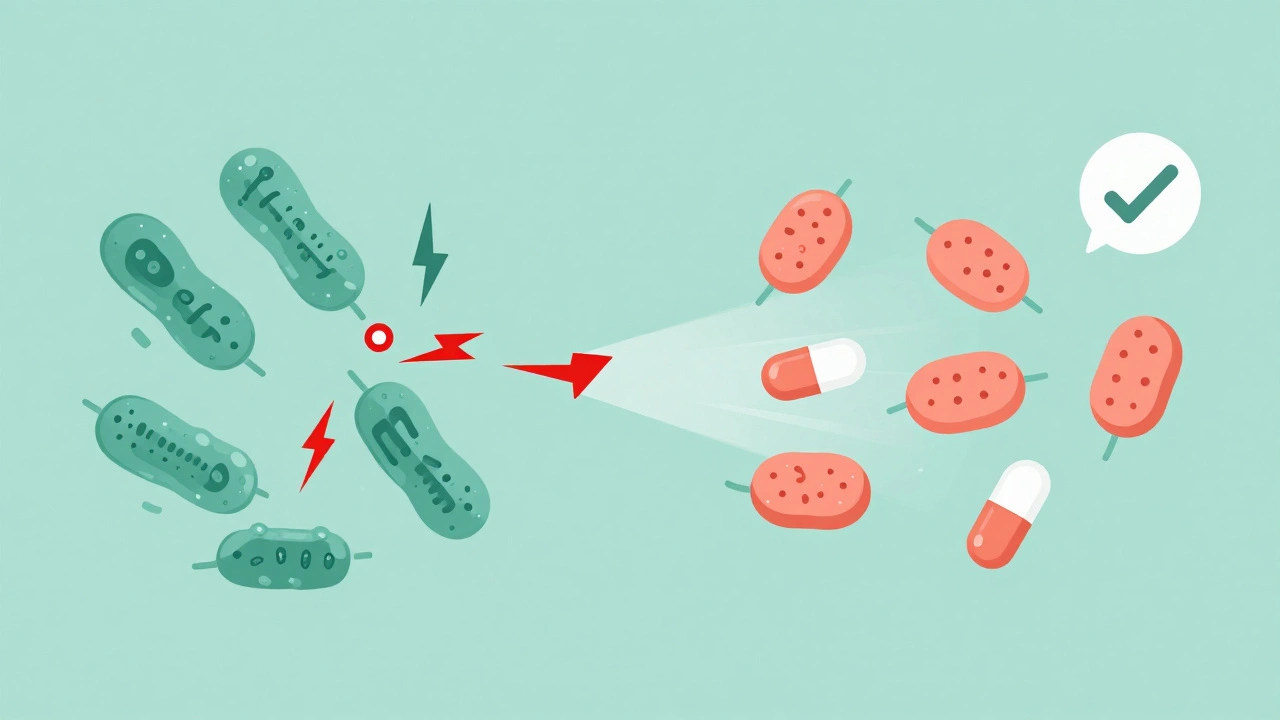
When to Start - and When to Stop
Don’t wait until you feel sick to start. Probiotics work best when you start early. The best window? Within 48 hours of your first antibiotic dose. Studies show that people who start within two days reduce their diarrhea risk by 71% compared to those who wait. And don’t stop when the antibiotics run out. Your gut is still recovering. Continue taking probiotics for at least 7-14 days after your last antibiotic pill. Some studies show that people who kept going for 14 days had 89% better microbiome recovery than those who stopped early. Think of it like rebuilding a house after a storm. The antibiotics tore it down. The probiotics help lay the bricks back. But you can’t stop after one day. You need time.What Happens If You Forget?
Life gets busy. You’re at work. You’re running late. You skip your probiotic. It happens. But skipping doses cuts effectiveness by 37%, according to clinical studies tracking stool samples. If you miss one, don’t double up. Just get back on track with your next scheduled dose. Consistency matters more than perfection. If you’re taking probiotics with meals, that’s fine - just keep the two-hour gap from your antibiotic. Many people find it easiest to take probiotics with breakfast and dinner, and antibiotics in between.What About Probiotic Foods?
Yogurt, kefir, sauerkraut - they’re great. But they’re not a substitute for supplements during antibiotic treatment. Why? The dose is too low. A serving of yogurt might have 1-2 billion CFUs. You need 10-20 billion. Plus, the strains in food aren’t always the ones proven to work with antibiotics. Stick to supplements for the duration of your treatment. You can enjoy fermented foods afterward to support long-term gut health.
The Biggest Mistake People Make
Taking probiotics and antibiotics at the same time. It’s the #1 error. People think, “I’m taking both, so it’s better.” But it’s the opposite. You’re killing the good guys before they can help. Another mistake? Choosing a probiotic without checking the strain. Many bottles just say “probiotic blend” with no names listed. That’s a red flag. You can’t know if it’s effective if you don’t know what’s in it. Look for specific strain names on the label - like Lactobacillus rhamnosus GG or Saccharomyces boulardii CNCM I-745. And don’t assume more strains = better. The science says otherwise. One proven strain at the right dose beats a mystery mix.What’s Next? The Future of Probiotics
Science is moving fast. Companies are now making time-release capsules that protect probiotics from antibiotics. Some are even testing personalized probiotics based on your gut microbiome. But right now, those are still in research labs. For now, the rules haven’t changed. Two hours. The right strain. The right dose. Consistent timing. That’s your playbook. The CDC’s 2024 antimicrobial resistance report confirms that 27 out of 31 major medical institutions still recommend the two-hour spacing rule as standard care. That’s not outdated advice. It’s the most tested, proven, and reliable method we have.Quick Recap: Your Probiotic-antibiotic Game Plan
- Start probiotics within 48 hours of your first antibiotic dose.
- Take probiotics at least 2 hours before or after your antibiotic.
- Use Lactobacillus rhamnosus GG or Saccharomyces boulardii - they’re the most effective.
- Dose: 10-20 billion CFUs for most adults on antibiotics.
- Keep taking probiotics for 7-14 days after antibiotics end.
- Yeast probiotics (like S. boulardii) can be taken at the same time as antibiotics.
- Check the label. If strain names aren’t listed, skip it.
- Don’t double up if you miss a dose. Just get back on schedule.
Antibiotics save lives. But they don’t have to wreck your gut. With the right timing, you can protect your microbiome without giving up the medicine you need.





11 Comments