Surviving a heart attack is just the beginning. The real work starts when you leave the hospital. Your heart was damaged, and your body needs time to heal-but healing doesn’t mean sitting still. It means moving forward, carefully and consistently, with the right medications, the right food, and the right amount of activity. Rushing this process can lead to another heart attack. Skipping it can cost you your life. This isn’t about getting back to normal. It’s about building a new normal-one that keeps your heart strong for years to come.
Medications: Your Lifeline After the Attack
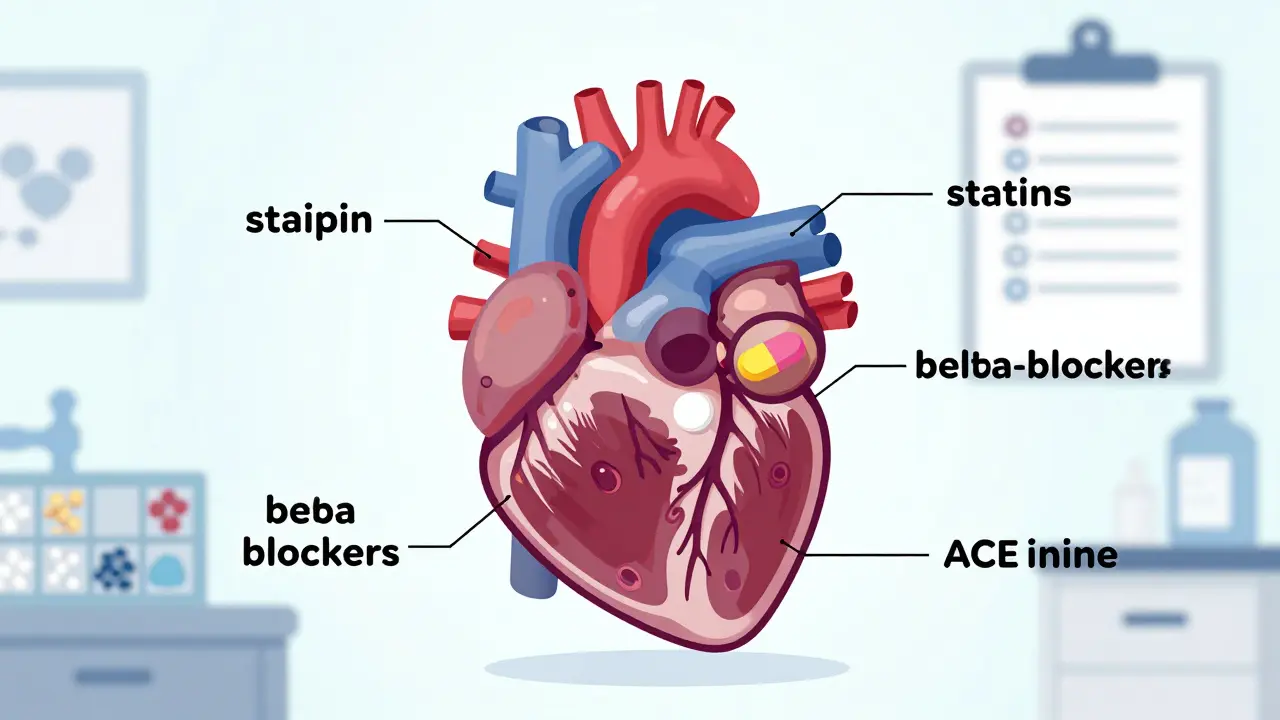
Right after your heart attack, your doctors start you on a stack of medicines. Some you’ve never heard of. Others you’ve taken before, but now they’re doing something different. These aren’t optional. They’re not just to make you feel better. They’re to stop your heart from breaking again.
Common meds include aspirin to thin your blood, statins to lower cholesterol, beta-blockers to slow your heart rate and reduce strain, and ACE inhibitors or ARBs to lower blood pressure and help your heart heal. If you had a severe blockage or abnormal heart rhythms, you might also get antiplatelets or antiarrhythmics. Your pharmacist will explain what each one does. Write it down. Keep a list in your wallet. Carry it with you everywhere-even to the grocery store.
Never skip a dose because you feel fine. Feeling good doesn’t mean your heart is healed. It means the medicine is working. If you get side effects-dizziness, fatigue, nausea-don’t stop. Call your doctor. There’s often another pill that works just as well without the problem. And if you’re on ten different pills, don’t panic. That’s normal. Cardiac rehab teams have special programs to help you manage them. Some even offer blister packs with doses labeled by day and time.
Diet: Food That Heals, Not Hurts
After a heart attack, your plate becomes your medicine cabinet. You don’t need fancy diets or expensive superfoods. You need simple, consistent changes.
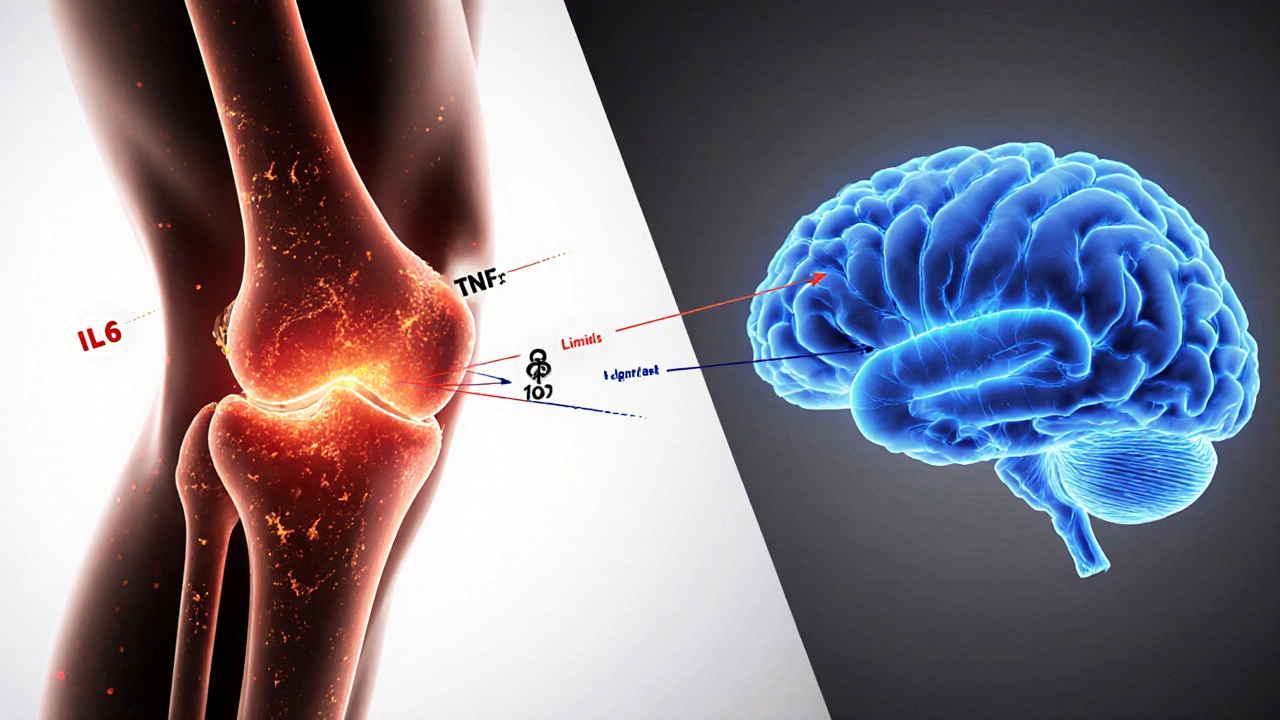
Start by cutting out processed foods-packaged snacks, frozen meals, sugary drinks, and anything with trans fats. These raise bad cholesterol and inflammation, both of which clog your arteries. Replace them with vegetables, fruits, whole grains, beans, nuts, and fatty fish like salmon or mackerel. These foods are rich in fiber, omega-3s, and antioxidants that help your heart repair itself.
Watch your sodium. Too much salt raises blood pressure, and high blood pressure forces your heart to work harder. Aim for less than 1,500 mg a day. That’s about half a teaspoon of salt. Read labels. Canned soups, bread, and even breakfast cereals can hide salt. Cook at home. Use herbs, garlic, lemon, and vinegar instead of salt for flavor.
Portion control matters too. Even healthy foods can hurt if you eat too much. A serving of meat is the size of your palm. A serving of pasta is half a cup-about the size of a tennis ball. A dietitian from your cardiac rehab program will help you build meals that fit your culture, your taste, and your health needs. They won’t take away your favorite foods. They’ll help you make them safer.
Activity: Moving Back to Life
You’re tired. You’re scared. You don’t want to move. That’s normal. The first week home, you might feel weak just walking to the bathroom. Your heart muscle is healing. It needs rest.
But rest doesn’t mean lying on the couch all day. Light movement is key. Walk around your house. Go up and down the stairs slowly. Sit in a chair and wiggle your feet. These small actions keep your blood flowing and prevent clots.
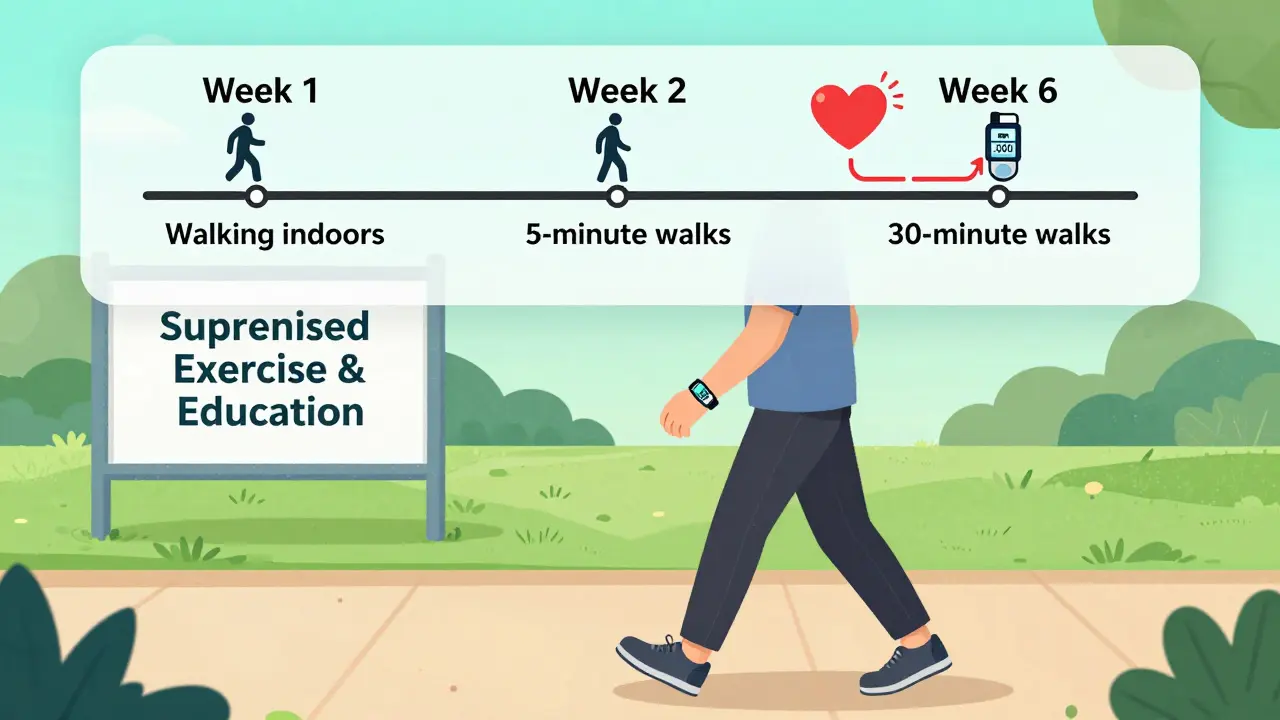
By week two or three, most people can start walking outside for 5 to 10 minutes at a time. Build up slowly. Add a minute each day. Walk with a friend. Use a pedometer. Aim for 30 minutes total a day, broken into smaller chunks if needed. The goal isn’t speed. It’s consistency.
Cardiac rehab is where the real progress happens. These programs run three times a week for 8 to 12 weeks. You’ll do supervised exercise on a bike, treadmill, or elliptical. Your heart rate and blood pressure are monitored. You’ll learn how hard you can safely push. You’ll also get education on stress, sleep, and quitting smoking.
Don’t wait for your doctor to suggest it. Ask for it. Most insurance covers it. And studies show people who complete rehab are 25% less likely to have another heart attack or die from heart disease.

Cardiac Rehab: The Missing Piece
Many people think rehab is just exercise. It’s not. It’s a full reset. You’ll meet nurses, physiotherapists, dietitians, and counselors-all focused on helping you live longer and feel better.
In rehab, you’ll learn how to recognize warning signs: chest pain that doesn’t go away, sudden shortness of breath, dizziness, or an irregular heartbeat. You’ll get a plan for what to do if they happen. You’ll also talk about anxiety and depression. It’s common to feel scared, guilty, or overwhelmed after a heart attack. Rehab gives you tools to cope. Group sessions help you realize you’re not alone.
And rehab isn’t just for the first few months. Many programs offer maintenance classes for life. Keep going. Even if you feel fine, your heart still needs support.
Follow-Up and Long-Term Thinking
You’ll have your first follow-up appointment 4 to 6 weeks after leaving the hospital. Your doctor will check your heart function, adjust meds, and review your progress. Don’t skip it. If you don’t feel like you’re improving, say so. If you’re still too tired to walk to the mailbox, that’s not normal. There’s help.
Long-term, your goal isn’t just to survive. It’s to thrive. That means checking your blood pressure and cholesterol regularly. Keeping your weight in a healthy range. Getting enough sleep. Managing stress through breathing, meditation, or walking. And never, ever going back to smoking.
Some risk factors can’t be changed-age, family history, gender. But the ones you can control? You have power over them. Every healthy meal, every walk, every pill taken on time, every time you say no to stress-that’s how you protect your heart.
When to Call for Help
You don’t have to guess when something’s wrong. Here’s when to call 911 or go to the ER:
- Chest pain that lasts more than a few minutes or comes and goes
- Shortness of breath that doesn’t improve with rest
- Sudden dizziness, fainting, or confusion
- Pain spreading to your jaw, neck, arm, or back
- Heartbeat that feels too fast, too slow, or irregular
If you’re unsure, call your doctor. Better safe than sorry. Your heart is still healing. Don’t risk it.
How long does it take to recover from a heart attack?
Recovery takes anywhere from two weeks to three months, depending on how severe the heart attack was and your overall health. Most people can return to light activities within a week or two, but full recovery-especially with exercise and stamina-takes months. The key is not to rush. Cardiac rehab programs help you progress safely.
Can I drive after a heart attack?
Usually, you can drive again after one to four weeks, but it depends on your symptoms and your doctor’s advice. If you had complications like fainting or irregular heart rhythms, you may need to wait longer. Always check with your healthcare provider before getting behind the wheel.
Do I need to take these medications forever?
For most people, yes. Medications like statins, beta-blockers, and aspirin are meant for long-term use because they prevent future heart damage. Stopping them-even if you feel fine-can trigger another heart attack. Always talk to your doctor before making changes.
Is it safe to have sex after a heart attack?
Yes, for most people. Sex is a moderate physical activity, similar to walking up two flights of stairs. If you can walk briskly without chest pain or shortness of breath, you’re likely ready. Talk to your doctor if you’re unsure. If you take nitrates for chest pain, don’t use erectile dysfunction drugs like Viagra-they can cause dangerous drops in blood pressure.
What if I can’t afford my medications?
Many pharmaceutical companies offer patient assistance programs. Pharmacies often have discount cards for common heart meds. Talk to your pharmacist or your cardiac rehab team-they know how to help you find low-cost or free options. Never skip doses because of cost. There’s always a solution.
Next Steps: What to Do Today
Right now, here’s what you can do:
- Call your doctor’s office and ask for a referral to cardiac rehab.
- Write down every medicine you’re taking, including dose and time.
- Plan your next meal: swap out processed carbs for vegetables and lean protein.
- Take a 5-minute walk outside-no rush, just movement.
- Write down one fear you have about your recovery. Bring it to your next appointment.
Recovery isn’t a race. It’s a rhythm. Slow, steady, and supported. Your heart has already survived the worst. Now it’s time to help it live well-for decades to come.





15 Comments