Using a pill organizer seems simple-just sort your pills by day and time, right? But if you’re not careful, it can become a hidden danger. Every year, thousands of people accidentally overdose because they misused their pill organizer. It’s not the device itself that’s risky. It’s how people fill it, store it, and trust it without double-checking. The truth is, a pill organizer can save your life-or end it-depending on how you use it.
Why Pill Organizers Can Cause Overdoses
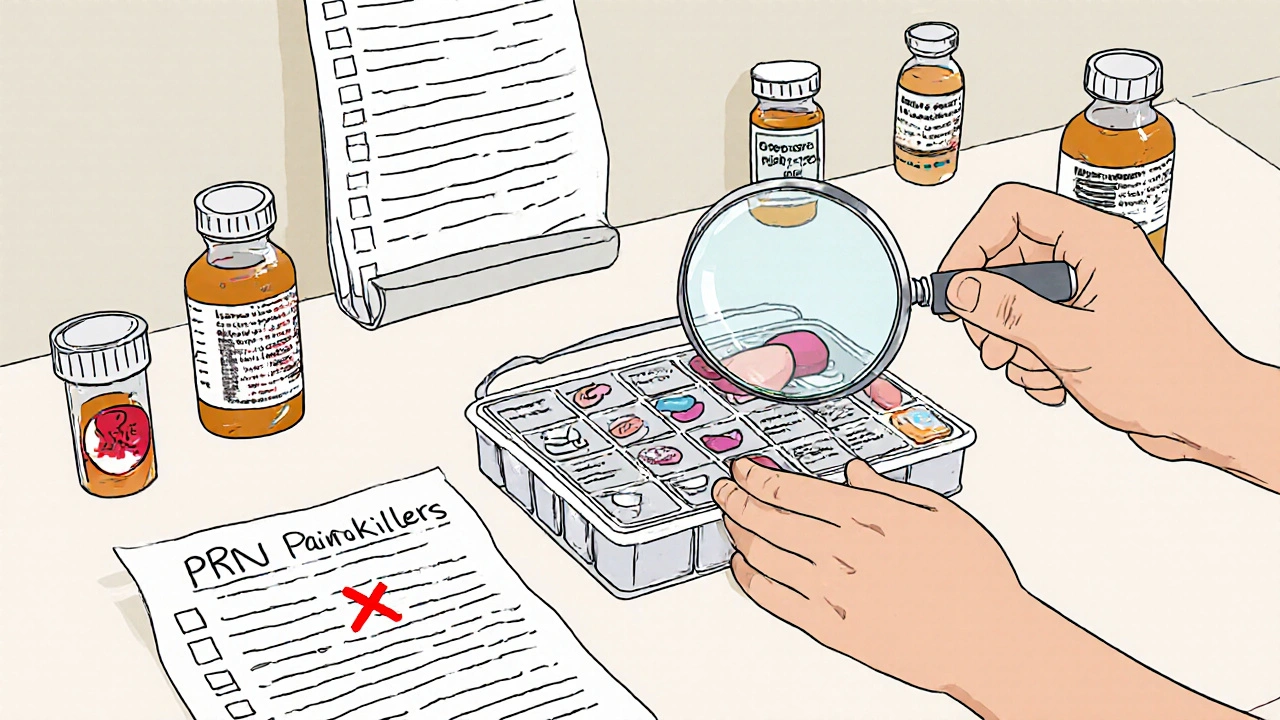
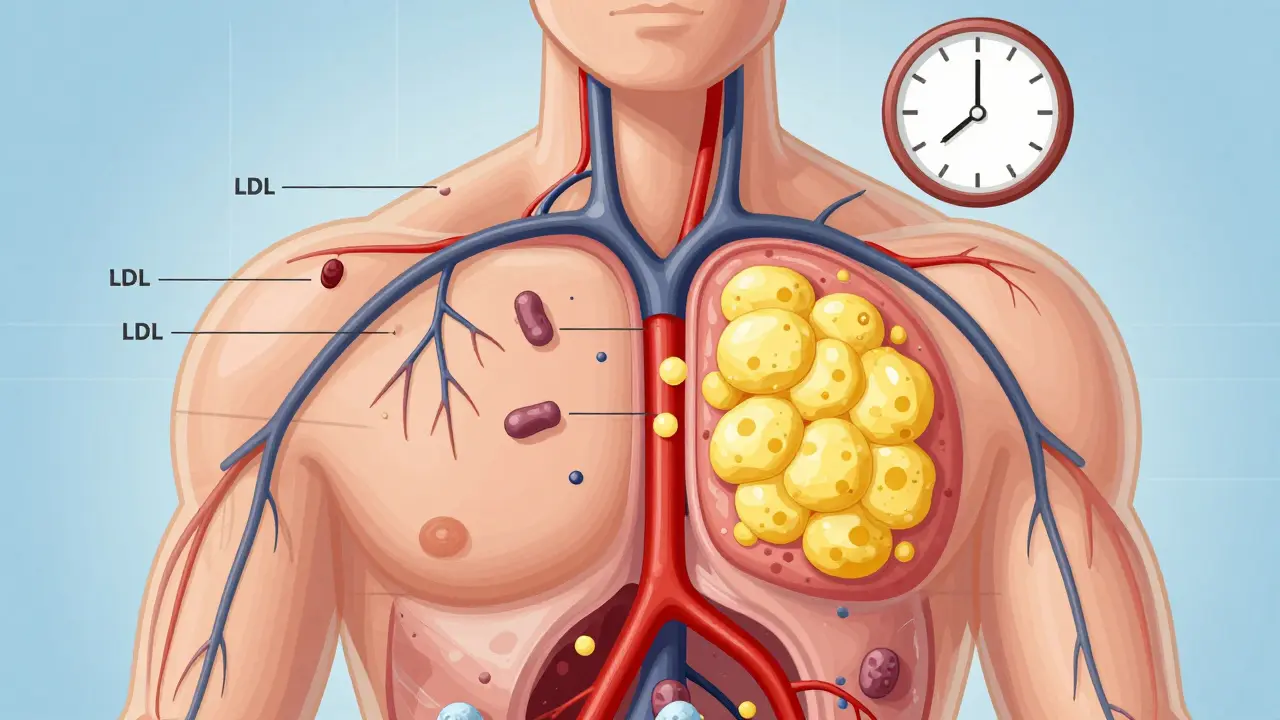
Pill organizers are designed to help you take the right medicine at the right time. But when used wrong, they make mistakes easier to make. A 2022 study in the Journal of the American Geriatrics Society found that improper use increases overdose risk by 23% in older adults. Why? Because people start treating their organizer like a magic box that knows what’s inside-instead of a tool that needs constant checking. The biggest mistake? Putting "as needed" (PRN) medications like painkillers or anti-anxiety pills into daily compartments. If you put hydrocodone or alprazolam in your Monday morning slot, you might take it even if you don’t need it. That’s how people end up taking two or three doses in one day. In fact, 38% of all accidental overdoses linked to pill organizers happen because PRN meds were mixed in with scheduled ones. Another big problem is outdated labels. People refill their organizer using old pill bottles instead of their current medication list. If your doctor changed your dose last month but you’re still using last year’s bottle, you’ll fill your organizer with the wrong amount. WebMD reports that 28% of medication errors come from this exact mistake.What Medications Should NEVER Go in a Pill Organizer
Not all pills are safe to put in a pill box. Some need special handling. Here’s what to keep out:- Liquid medications-they leak, mix, and ruin other pills.
- Refrigerated drugs-like insulin or some antibiotics-lose potency if stored at room temperature.
- Chewable, dissolvable, or soft gel capsules-they stick together, break apart, or crumble.
- Medications that degrade in humidity-like nitroglycerin or some seizure drugs-can become useless or dangerous if stored in the bathroom.
How to Fill a Pill Organizer the Right Way
There’s a proven, step-by-step method used by hospitals and pharmacists to avoid mistakes. Follow this every time you refill:- Wash your hands with soap for at least 20 seconds. Dirty hands can contaminate pills or transfer residue between medications.
- Gather everything-your current medication list (from your doctor or pharmacy), all pill bottles, your organizer, and a clean surface.
- Check your list against your bottles. Are the names, doses, and instructions the same? If not, call your pharmacy before filling anything.
- Fill one medication at a time. Don’t dump all your pills into a pile. Take one drug, count the correct number, place it in the right compartment, then move to the next. This cuts double-dosing errors by 63%, according to Memorial Sloan Kettering.
- Verify each compartment. Look at the pill, read the bottle label again, then check the organizer. Do they match? If not, stop and figure out why.
- Keep original bottles nearby. Never toss them. You’ll need them to double-check when you’re unsure.

Storage and Maintenance Matter More Than You Think
Where you keep your pill organizer is just as important as how you fill it.- Store it in a cool, dry place-like a bedroom drawer or kitchen cabinet.
- Avoid heat and humidity. Don’t put it near the stove, radiator, or bathroom.
- Keep it out of reach of children and pets. Use organizers with child-resistant locks if you have young kids around.
- Replace your organizer every 6 to 12 months. Plastic compartments crack, labels fade, and lids get loose. A 2023 National Council on Aging study found 28% of seniors use organizers older than five years-with degraded compartments that leak or misalign.
Use Alarms and Tracking to Stay Safe
Your phone is a powerful tool for medication safety. Set alarms 15 minutes before each dose. That gives you time to grab the right pill, check the label, and take it calmly. Studies show this reduces verification errors by 44%. If you’re managing more than five medications, consider an electronic organizer with alarms and compartment tracking. These devices cost $25 to $100 and can alert you if you open a compartment too soon or too often. Hero Health’s 2023 software update now triggers overdose warnings if someone opens the same compartment twice in four hours. Some pharmacies now offer free organizer filling services with pharmacist verification. In 2023, 68% of U.S. pharmacies started offering this. It’s free, takes 10 minutes, and cuts errors by 52%. Ask your pharmacist if they do it.What to Do If You’re Unsure
If you’ve ever looked at your organizer and thought, "Wait, is this the right pill?"-you’re not alone. Nearly one in three accidental overdoses happen because people didn’t verify what was inside. Here’s what to do:- Stop. Don’t take it.
- Find the original bottle.
- Compare the pill’s color, shape, and imprint code (the letters/numbers on it).
- If it still doesn’t match, call your pharmacy. They can identify pills by image or code.

When to Upgrade Your Organizer
Not all organizers are created equal. If you’re still using a basic $3 plastic box with no labels, it’s time to upgrade.- For simple regimens (once or twice daily): A 7-day, 2-compartment organizer ($7-$12) works fine.
- For complex regimens (three or four times daily): Get a 7-day, 4-compartment box with clear labels for AM, noon, PM, bedtime.
- For memory issues or vision problems: Look for Braille labels, large print, or color-coded compartments.
- For high-risk meds (opioids, sedatives): Use a smart organizer with alerts and locking features.
Real Stories, Real Mistakes
On Reddit’s r/MedicationAdherence, users shared 142 overdose incidents in 2023. The top three causes:- Putting PRN painkillers in daily slots (58 cases)
- Not updating the organizer after a prescription change (49 cases)
- Mixing meds that shouldn’t be stored together (35 cases)
Final Rule: Never Trust the Box
Your pill organizer is a helper-not a guardian. It can’t tell you if a pill is expired, if your dose changed, or if you already took it. Only you can do that. Always verify. Always check. Always keep the original bottles. And if you’re ever unsure, don’t guess-call your pharmacist. They’re paid to catch mistakes before they happen.Medication safety isn’t about having the fanciest organizer. It’s about building habits that protect you. One step at a time.
Can I put all my pills in one organizer?
No-not all pills are safe to store together. Avoid putting liquids, refrigerated meds, chewables, or soft gels in a pill box. Also, never mix "as needed" meds like painkillers or anxiety pills with your daily schedule. Keep those separate and only take them when you truly need them.
Is it safe to store my pill organizer in the bathroom?
No. Bathrooms are too humid. Steam from showers can damage pills, making them less effective or even dangerous. Store your organizer in a cool, dry place like a bedroom drawer or kitchen cabinet instead.
How often should I refill my pill organizer?
Most people refill weekly-pick one day, like Sunday morning, and stick to it. This builds a routine. Always check your current medication list before refilling. Never refill from old pill bottles; always use your latest prescription list.
What should I do if I think I took the wrong pill?
Stop. Don’t take any more pills. Find the original bottle and compare the pill’s color, shape, and imprint code. If it doesn’t match, call your pharmacy immediately. They can identify pills by image or code. If you’ve already taken a wrong dose, contact your doctor or poison control right away.
Are smart pill organizers worth the cost?
If you take four or more medications, have memory issues, or have had a near-miss overdose, yes. Smart organizers with alarms, locks, and usage tracking can reduce errors by up to 33%. Medicare covers them for qualifying beneficiaries. Even basic models with alarms are worth it if you often forget doses.






12 Comments