Standing up from a chair and feeling dizzy? For older adults on blood pressure medication, this isn’t just a minor inconvenience-it’s a warning sign. Orthostatic hypotension, a sudden drop in blood pressure when standing, affects up to 26% of hypertensive seniors. And here’s the twist: the very drugs meant to protect their hearts might be making them more likely to fall.
Why Older Adults Are at Higher Risk
As we age, our bodies change in ways that make blood pressure control harder. The baroreflex, which normally tells your heart and blood vessels to adjust when you stand, becomes sluggish. Blood vessels stiffen. Kidneys produce less renin, a hormone that helps maintain pressure. These changes mean even small drops in blood pressure can cause dizziness, blurred vision, or fainting.It’s not just aging alone. Many seniors take multiple medications. A study from the Irish Longitudinal Study on Ageing found that nearly one in four older adults with high blood pressure also experience orthostatic hypotension. The risk climbs with age, especially after 70. And here’s what most doctors didn’t used to realize: treating high blood pressure aggressively doesn’t necessarily make orthostatic hypotension worse.
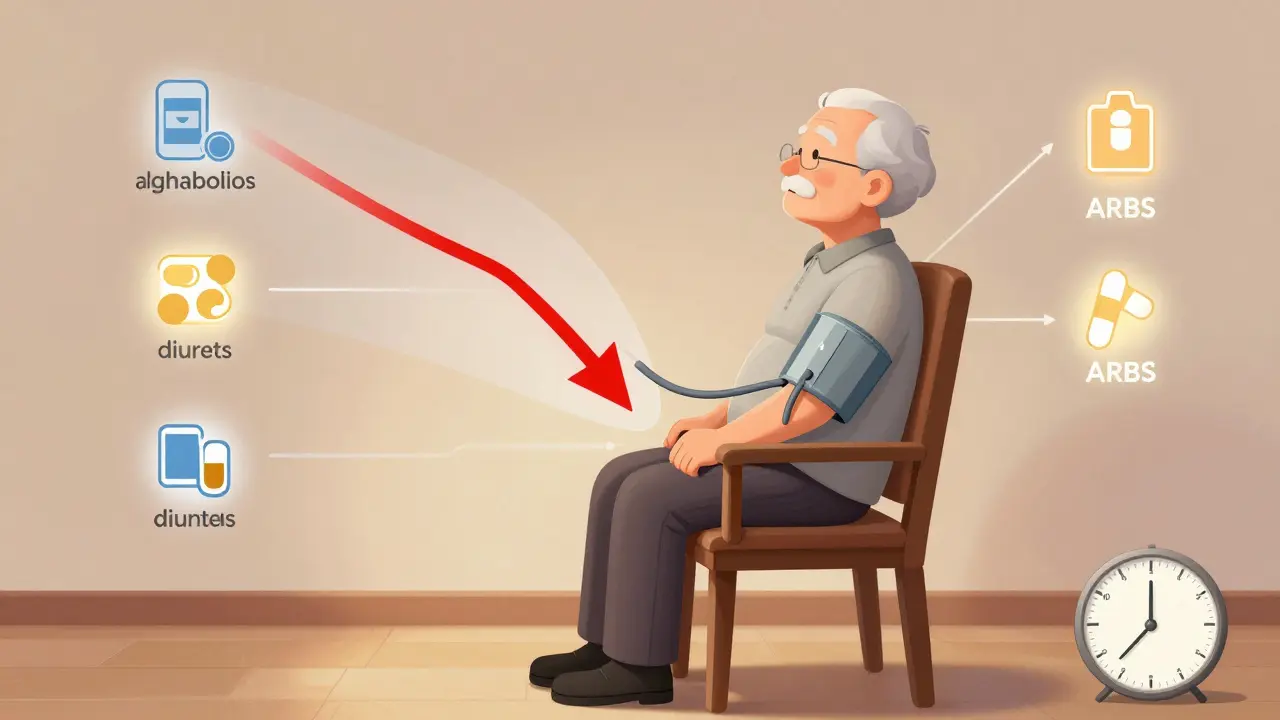
Which Blood Pressure Medications Are Riskiest?
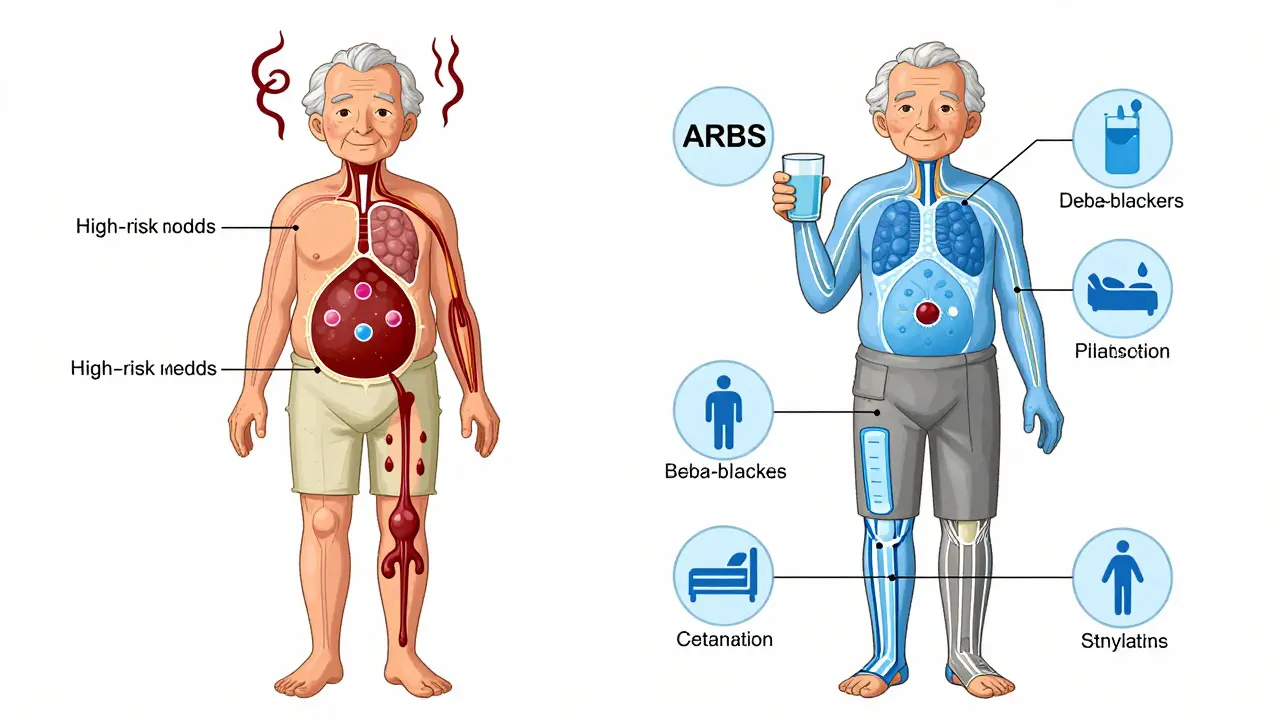
Not all antihypertensives are created equal when it comes to orthostatic risk. Some are far more likely to cause problems than others.- Alpha blockers (like doxazosin, terazosin): These carry the highest risk-up to 28% of seniors on these drugs develop orthostatic hypotension. They’re often prescribed for prostate issues, but their effect on blood vessels is too strong for many older bodies.
- Beta-blockers (like metoprolol, atenolol): These reduce heart rate and force, which can make it harder to compensate when standing. Studies show a 3.36x higher risk of sustained low blood pressure after standing.
- Diuretics (like furosemide, hydrochlorothiazide): By flushing out fluid, they reduce blood volume. This can cause a sharp drop in pressure when standing, especially if taken too late in the day.
- Central sympatholytics (like clonidine): These slow down the nervous system’s ability to raise blood pressure, making standing dangerous.
- Calcium channel blockers (like amlodipine): Risk varies. Amlodipine and lacidipine are better tolerated because they act slowly. But diltiazem and verapamil, which are metabolized slower in older adults, can still cause problems in the first few months.
On the other end of the spectrum, ACE inhibitors (like lisinopril) and ARBs (like losartan) are the safest choices. Multiple studies show they’re linked to 14-15% lower rates of orthostatic hypotension compared to other classes. Some research even suggests they may help prevent it.
The Big Myth: More Aggressive Treatment = More Danger
For years, doctors assumed that pushing blood pressure lower-say, below 120 mm Hg-would increase falls and dizziness in older patients. That’s what the SPRINT trial changed.In this landmark study, over 9,000 adults over 50 with high blood pressure were split into two groups: one aimed for a systolic pressure under 120, the other under 140. After three years, the intensive group had 25% fewer heart attacks, strokes, and heart failure cases. And guess what? Their rate of orthostatic hypotension was almost identical: 14.7% vs. 14.5%. No increase. No extra falls.
That’s because the real danger isn’t low standing pressure-it’s high lying pressure. When someone has uncontrolled high blood pressure while lying down, it strains the heart and arteries. Lowering that pressure reduces overall cardiovascular risk, even if standing pressure dips slightly. As Dr. Harry Goldblatt from Case Western Reserve put it: "The impetus of adverse events is supine/seated hypertension, not the standing BP."
What to Do If You’re Already on Risky Medication
If you or a loved one is on a high-risk drug and experiencing dizziness when standing, don’t stop abruptly. Talk to your doctor. Here’s what a smart plan looks like:- Review every medication. Ask: Is this still necessary? Are there safer alternatives? The American Geriatrics Society Beers Criteria lists alpha blockers, certain beta-blockers, and clonidine as potentially inappropriate for seniors with orthostatic hypotension.
- Switch to lower-risk drugs. If you’re on doxazosin, ask about switching to an ARB like losartan. Studies show 65% of patients report less dizziness and fewer falls after switching.
- Time your doses. Take diuretics and long-acting meds no earlier than 3 hours before bed. This avoids nighttime lows and morning spikes.
- Monitor standing pressure. Your doctor should check your blood pressure after you’ve been lying down for 5 minutes, then again after standing for 1 and 3 minutes. That’s the only way to catch orthostatic hypotension.
Non-Drug Strategies That Actually Work
Medication changes help-but they’re not the whole story. Simple lifestyle tweaks can cut dizziness in half.- Stand up slowly. Don’t jump out of bed. Sit on the edge for 30 seconds. Then stand still for another 30 seconds before walking.
- Hydrate before standing. Drink a glass of water before getting up, especially after meals or bathroom trips. Fluid helps maintain volume.
- Wear compression stockings. These help push blood back up from the legs. Studies show they reduce symptoms in over half of patients.
- Avoid hot showers and long baths. Heat dilates blood vessels and can trigger a drop in pressure.
- Elevate the head of your bed. Raising the head 6-10 inches helps reduce nighttime high pressure and improves morning stability.
Most people see improvement within 2-4 weeks of making these changes. The Cleveland Clinic says orthostatic hypotension rarely causes long-term damage if managed properly.
What About Medications Just for Orthostatic Hypotension?
Sometimes, lifestyle and switching drugs aren’t enough. In those cases, doctors may prescribe drugs that raise standing pressure:- Midodrine (Orvaten): A vasoconstrictor that tightens blood vessels. Works well but can cause scalp tingling or supine hypertension.
- Droxidopa (Northera): Converts to norepinephrine to boost pressure. Requires careful dosing.
- Fludrocortisone: A steroid that increases salt and water retention. Risk of swelling and high lying pressure.
- Pyridostigmine (Mestinon): Helps nerves signal blood vessels to constrict. Less commonly used but effective for some.
These aren’t first-line treatments. They’re for patients who still have symptoms after optimizing their blood pressure meds and lifestyle. Side effects are real, and they’re not risk-free.
The Future: Smarter Drugs and Personalized Care
The field is changing fast. Two new drugs are in Phase II trials that only activate when you stand up-releasing medication only during posture changes, not while lying down. That could eliminate the dizziness without sacrificing heart protection.Also, the European Society of Cardiology is finalizing new guidelines for managing hypertension in patients with orthostatic hypotension, due out in late 2024. And the OPTIMISE trial is testing whether targeting a systolic pressure of 130-140 mm Hg is safer than lower goals for seniors with OH.
Meanwhile, prescribing trends are already shifting. In 2023, 38% of new hypertension prescriptions for seniors were ACE inhibitors or ARBs-up from 32% in 2020. That’s because doctors are finally catching on: the safest way to protect an older heart isn’t to hold back-it’s to choose the right drugs and manage them wisely.
Key Takeaways
- Orthostatic hypotension affects up to 26% of older adults on blood pressure meds-but it’s often preventable.
- Alpha blockers, beta-blockers, and diuretics carry the highest risk. ACE inhibitors and ARBs are safest.
- Aggressive blood pressure control does NOT increase orthostatic hypotension risk-it may reduce it.
- Always check standing blood pressure. Don’t assume symptoms are "just aging."
- Non-drug strategies (slow standing, hydration, compression socks) work better than most people think.
- Never stop meds cold turkey. Work with your doctor to switch or adjust safely.
Is orthostatic hypotension normal as you get older?
No, it’s not a normal part of aging. While the risk increases with age due to physiological changes, orthostatic hypotension is a medical condition that should be evaluated and treated. It’s often caused or worsened by medications, dehydration, or other health issues-not just getting older.
Can I stop my blood pressure medicine if I feel dizzy when standing?
Never stop abruptly. Stopping suddenly can cause dangerous spikes in blood pressure, increasing your risk of stroke or heart attack. Instead, talk to your doctor. They can check if your medication is the cause and safely switch you to a lower-risk option.
Which blood pressure meds are safest for seniors with dizziness on standing?
ACE inhibitors (like lisinopril) and ARBs (like losartan) have the lowest risk of causing orthostatic hypotension. Calcium channel blockers like amlodipine and lacidipine are also generally well-tolerated. Avoid alpha blockers like doxazosin and certain beta-blockers unless absolutely necessary.
How long does it take to adjust after switching blood pressure meds?
It usually takes 4-6 weeks for your body to fully adjust after switching medications. During this time, your doctor will monitor your blood pressure both lying down and standing. Non-drug changes like slow standing and hydration can help speed up improvement.
Do compression stockings really help with dizziness when standing?
Yes. Studies show that compression stockings help reduce blood pooling in the legs, which improves circulation when standing. About 50-60% of seniors with orthostatic hypotension report fewer dizziness episodes after using them daily. They’re a simple, drug-free tool that works.
Next Steps for Seniors and Caregivers
If you’re managing blood pressure in an older adult:- Ask the doctor to check standing blood pressure at every visit.
- Keep a log: note when dizziness happens, what meds were taken, and what you were doing.
- Review all medications annually with a pharmacist or geriatrician.
- Encourage slow movements-especially after meals, naps, or using the bathroom.
- Install grab bars in the bathroom and remove tripping hazards at home.
Orthostatic hypotension doesn’t have to mean a life of falls and fear. With the right meds, smart habits, and a little patience, most seniors can stay steady on their feet-and protected from heart attacks and strokes at the same time.