When you hear the word generic, you probably think of cheap pills-same active ingredient, same effect, way cheaper. But when it comes to biologic drugs, things aren’t that simple. Biosimilars aren’t generics. They’re not exact copies. And yet, they’re still saving patients and health systems billions every year.
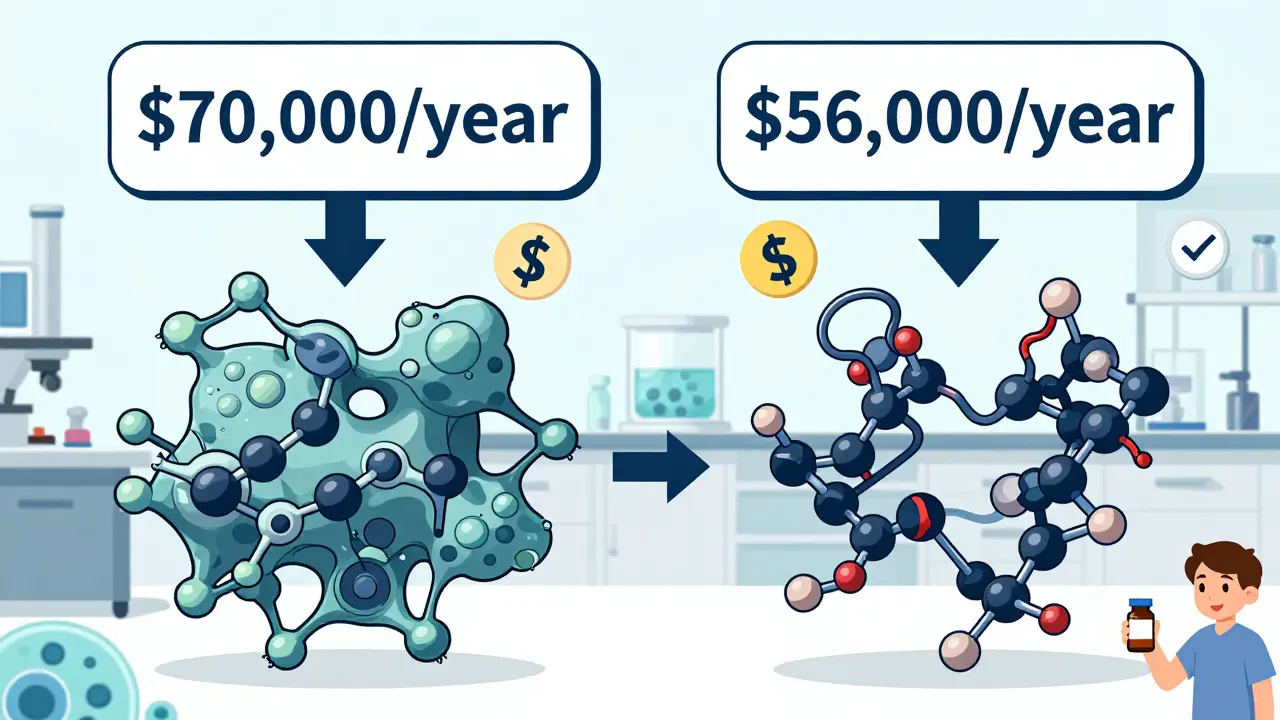
Biologics are complex drugs made from living cells. They treat serious conditions like rheumatoid arthritis, Crohn’s disease, cancer, and psoriasis. Because they’re so hard to make, they’re also incredibly expensive. Humira, for example, used to cost over $70,000 a year per patient in the U.S. Before biosimilars came along, there was no real competition. That meant prices stayed high, and many patients couldn’t afford them.
Then came biosimilars. These are highly similar versions of biologics, approved after years of testing to prove they work just as safely and effectively. The first one got FDA approval in 2015. Since then, the market has slowly but steadily changed. And the savings? They’re real.
How Much Do Biosimilars Actually Save?
In 2024, biosimilars saved the U.S. healthcare system $20.2 billion. That’s not a guess. That’s from a report by the Association for Accessible Medicines and IQVIA. Since 2015, the total savings have reached $56.2 billion. That’s money that went back into the system-money that let more people get treatment, or helped fund other critical care.
But here’s the catch: biosimilars don’t slash prices like generics do. Generic pills can drop 80-90% in price once they hit the market. Biosimilars? They usually land at 15-35% below the original biologic’s list price. That might sound modest. But when you’re talking about drugs that cost $60,000 a year, even a 20% cut means $12,000 saved per patient.
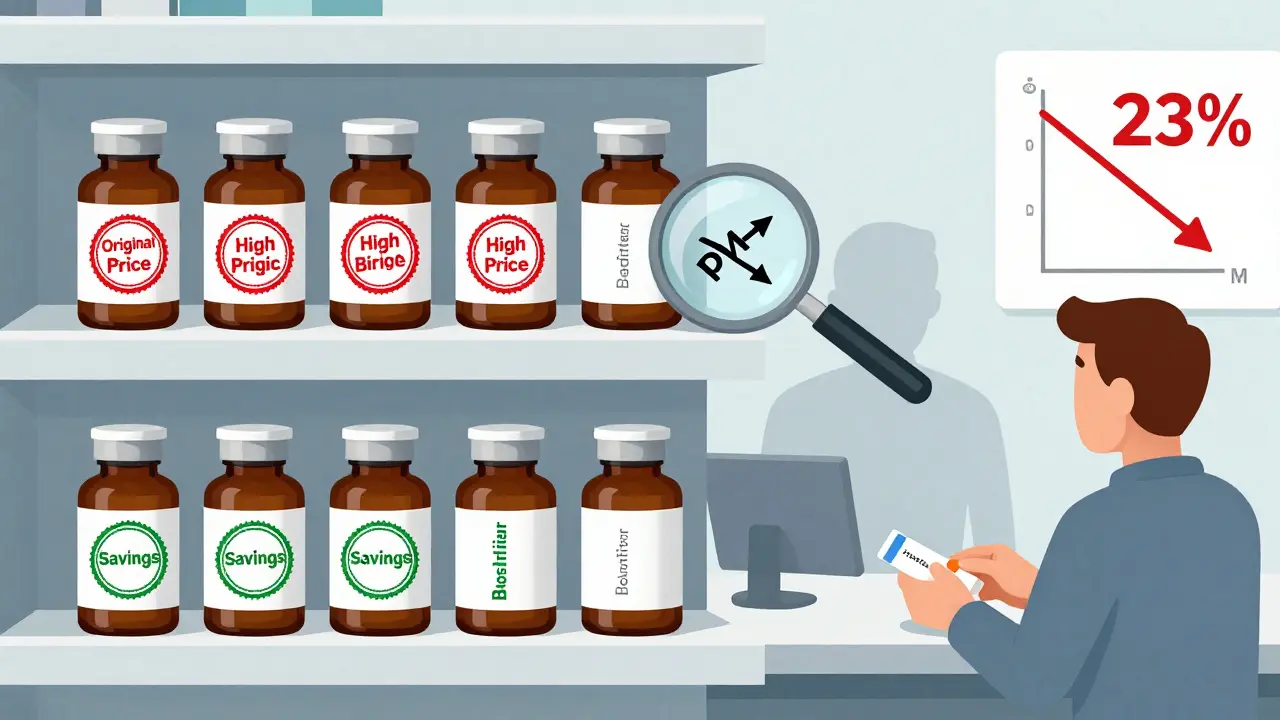
Take Humira. As of January 2025, 10 biosimilars were approved in the U.S., with several labeled as "interchangeable"-meaning pharmacists can swap them without a doctor’s permission. On list price alone, some of these biosimilars sold for up to 85% less than the original. That’s huge. But list price isn’t what patients pay. Rebates, discounts, and pharmacy benefit manager deals muddy the waters. The actual savings at the pharmacy counter? Around 23% lower out-of-pocket costs for patients using biosimilars, according to CSRxP data from 2025.
For Stelara, another top-selling biologic, biosimilars entered the market in mid-2024 with prices as low as 90% below the original. That’s the kind of drop that can turn a drug from unaffordable to accessible.
Why Don’t Biosimilars Save More?
It’s not that biosimilars aren’t working. It’s that the system isn’t set up to let them.
Biologics are made in living cells-think yeast, hamster ovary cells, or human cell lines. Every batch is slightly different. That’s why biosimilars can’t be exact copies. They have to be "highly similar" with no clinically meaningful differences. That complexity means development costs are huge-hundreds of millions of dollars. So manufacturers can’t afford to slash prices the way generic makers can.
Then there’s the rebate trap. Big drugmakers like AbbVie (maker of Humira) offer deep discounts to pharmacy benefit managers (PBMs) and insurers. These rebates can make the net price of the original biologic almost the same as the biosimilar’s list price. So even though the biosimilar is cheaper on paper, the rebate system keeps the originator in the driver’s seat. Pharmacies and insurers often stick with the original because the rebate makes it profitable for them-even if it costs patients more.
And here’s another problem: only 12 biologics have biosimilars in development right now. But over the next 10 years, 118 biologics are set to lose patent protection. That means 90% of upcoming opportunities for cost savings? Left untouched. That’s a $234 billion gap in potential savings.
In Europe, biosimilars have taken off faster. Countries like Norway now have biosimilar market shares over 85% for some drugs. Why? Because they use policies that encourage switching-like mandatory substitution and price caps. The U.S. doesn’t have those.
Who’s Saving Money-And How?
It’s not just patients. Employers are saving too.
Workspan Daily reported that if every employee switched from a biologic to its biosimilar, an employer could save an average of $1.53 million per year. Across all self-insured U.S. companies, switching just two biologics to biosimilars could save $1.4 billion annually.
Medicare Part B has seen consistent price erosion after biosimilars enter the market. As more biosimilars come in, the original drug’s price drops-even if it’s still being prescribed. That’s called price competition. It’s not direct. But it’s real.
Patients aren’t just paying less out of pocket. They’re getting access. Since 2015, biosimilars have enabled over 460 million extra days of therapy. That’s people who would’ve gone without treatment because of cost. That’s not just savings. That’s improved health outcomes.
What’s Holding Biosimilars Back?
Three things: confusion, complexity, and contracts.
Doctors and patients still worry that biosimilars aren’t as safe or effective. That’s not true. But it’s a myth that’s hard to shake. Education matters. So does transparency.
Pharmacy benefit managers (PBMs) often create formularies that favor their own private-label biosimilars or the original drug because of rebates. That limits competition. It’s not about what’s best for patients-it’s about what’s best for the middleman.
And contracts? They’re a maze. A biosimilar might have a lower list price, but if the originator offers a 50% rebate to a health plan, the net cost can be nearly identical. Without deep data analysis-like what Segal’s SHAPE platform provides-plans can’t see the real savings.
How to Get the Most Out of Biosimilars
If you’re an employer, insurer, or even a patient advocate, here’s what actually works:
- Push for formulary placement. Put biosimilars as the preferred option. Make them the first choice, not the backup.
- Use step therapy. Require patients to try the biosimilar before approving the originator. It’s not about denying care-it’s about starting with the most cost-effective option.
- Negotiate without rebates. Ask for transparent pricing. If you can get the biosimilar at a fixed price without rebate gimmicks, you’ll save more.
- Track utilization. Use data tools to see where biologics are being prescribed and where biosimilars are being underused.
- Educate providers and patients. Share real data. Show them studies. Tell them biosimilars aren’t "second-rate." They’re FDA-approved, safe, and effective.
It takes time. Usually 6 to 12 months to fully integrate biosimilar strategies into a health plan. But the payoff? Massive.
The Big Picture
Biologics are the most expensive part of the drug market. In 2023, they made up 98.9% of all biologic spending in the U.S. That’s down from 99.6% the year before. Slow progress. But progress.
Without biosimilars, we’d be stuck paying $70,000 a year for arthritis drugs. With them, we’re seeing prices drop by half, even three-quarters. Patients are getting treatment. Employers are saving money. Health systems are freed up to invest elsewhere.
But if we don’t fix the pipeline-don’t get more biosimilars approved for the next 118 biologics-we’re going to miss out on $234 billion in savings over the next decade. That’s not just a number. That’s thousands of lives. That’s better care for people with cancer, autoimmune diseases, and chronic conditions.
The science is there. The data is there. The savings are real. What’s missing is the will to change how we buy and use these drugs.
Are biosimilars as safe as the original biologics?
Yes. Before approval, biosimilars must undergo rigorous testing to prove they have no clinically meaningful differences in safety, purity, or effectiveness compared to the original. The FDA requires extensive clinical trials and data. Since 2015, over 3.3 billion days of patient therapy have been completed with biosimilars, with no unique safety concerns identified.
Why don’t biosimilars cost 80% less like generics?
Because biologics are made from living cells, not chemicals. Manufacturing them is like growing a complex organism-every batch is slightly different. This makes development and production far more expensive than making a generic pill. Biosimilars still need years of testing and specialized facilities, so savings are real but more modest-typically 15-35% below list price.
Do biosimilars lower out-of-pocket costs for patients?
Yes. In commercial insurance markets, patients using biosimilars pay, on average, 23% less out of pocket than those using the original biologic. For some drugs like Humira, out-of-pocket savings have ranged from 12% to 45%, depending on the plan and pharmacy.
Why are biosimilars still not widely used in the U.S.?
Three main reasons: rebate systems that favor originator drugs, lack of policy incentives to switch, and lingering misconceptions among doctors and patients. Even though biosimilars are cheaper and proven safe, PBMs and insurers sometimes keep the original drug on formularies because of hidden discounts.
What’s the "biosimilar void" and why does it matter?
The "biosimilar void" refers to the fact that 90% of biologics set to lose patent protection over the next decade have no biosimilars in development. That means $234 billion in potential savings could vanish. Without action, we’ll face the same high-price problems with new biologics-just like we did with Humira and Enbrel.




15 Comments