Acne doesn’t just annoy-it can make you feel invisible. If you’ve been prescribed Cleocin Gel (clindamycin), you’re not alone. Millions use it every year to calm red, inflamed breakouts. But after a few weeks, some people wonder: Is this really the best option? Maybe it’s not working as well as it should. Maybe your skin is getting irritated. Or maybe your doctor just ran out of samples and you’re stuck wondering what else is out there.
The truth? Cleocin Gel isn’t the only tool in the box. And depending on your skin type, how bad your acne is, or whether you’ve tried other treatments before, there might be something better suited to you. Let’s break down what Cleocin Gel actually does, how it stacks up against the most common alternatives, and who should consider switching.
What Cleocin Gel Actually Does
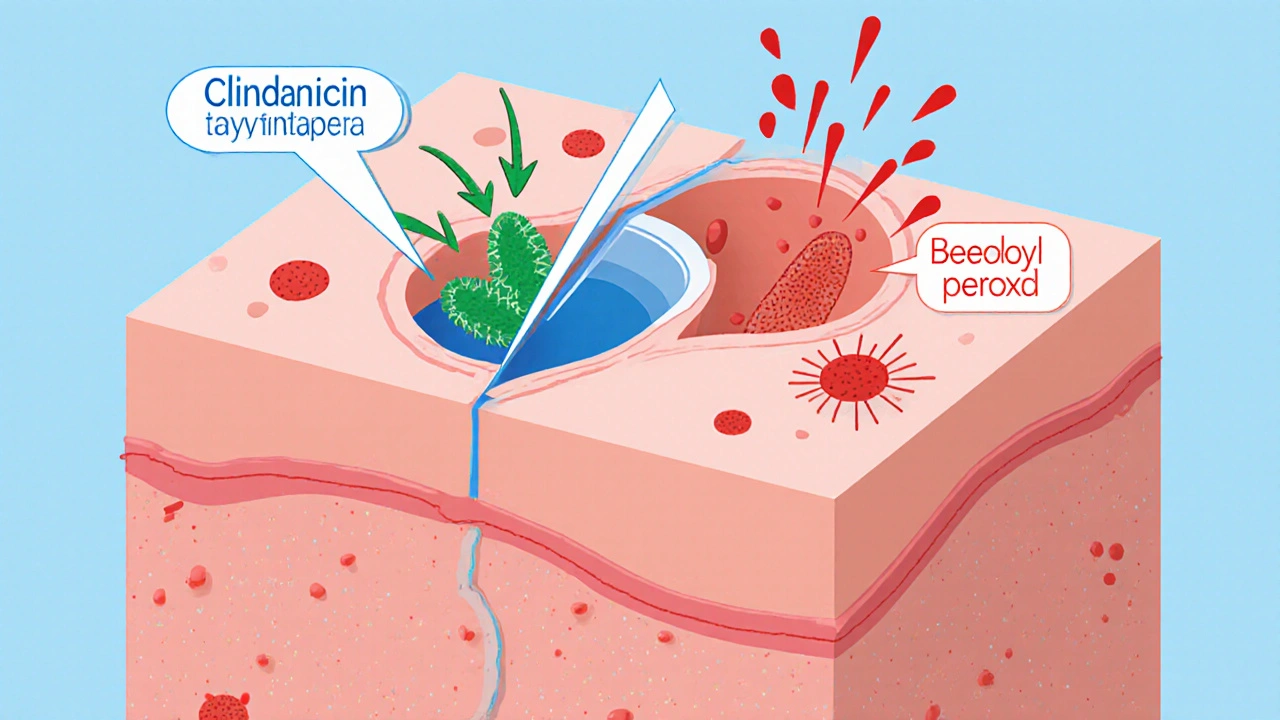
Cleocin Gel contains clindamycin phosphate, a topical antibiotic. It doesn’t dry out your skin like benzoyl peroxide. It doesn’t force cells to shed faster like retinoids. Instead, it targets the bacteria that cause acne-Propionibacterium acnes-right where they live: inside your pores. It also reduces inflammation, which is why it’s especially good for red, tender pimples and cystic breakouts.
It’s usually applied once a day, often in the evening. Most people start seeing results in 4 to 6 weeks. But here’s the catch: it doesn’t work for everyone. And over time, some strains of acne bacteria become resistant to clindamycin. That’s why dermatologists rarely recommend it alone anymore.
Why Cleocin Gel Alone Isn’t Enough Anymore
Back in the 2000s, doctors often prescribed clindamycin gel by itself. Now, guidelines from the American Academy of Dermatology say that’s outdated. Why? Because using a single antibiotic increases the chance of resistance. Studies show that after just 3 months of monotherapy, up to 50% of acne patients develop resistant bacteria.
That’s why Cleocin Gel is now almost always paired with another treatment-usually benzoyl peroxide. In fact, combination products like Clindamycin/Benzoyl Peroxide (Duac, Benzaclin) are now more common than plain clindamycin. These combos kill bacteria, reduce inflammation, and prevent resistance all at once.
If you’re still using Cleocin Gel alone, ask your doctor if switching to a combo product might help. It’s not about the gel being weak-it’s about how we use it.
Alternative #1: Benzoyl Peroxide (BPO)
Benzoyl peroxide is the OG acne fighter. It’s been around since the 1960s. It kills acne bacteria, unclogs pores, and reduces redness. Unlike antibiotics, bacteria can’t build resistance to it. That’s a huge plus.
It comes in 2.5%, 5%, and 10% strengths. Most people start with 2.5%-it’s just as effective as higher doses but causes way less dryness and peeling. You can find it in gels, washes, and creams. Some even combine it with clindamycin, which brings us back to why combo products are better.
Downside? It bleaches towels, pillowcases, and clothing. If you’re not careful, you’ll ruin your favorite black T-shirt. Also, it can be drying. But if your skin can handle it, it’s one of the most reliable options out there.
Alternative #2: Adapalene (Differin Gel)
If you’ve got blackheads, whiteheads, or clogged pores, adapalene is your best friend. It’s a retinoid-meaning it helps skin cells turn over faster so pores don’t get blocked. It also reduces inflammation, which makes it useful for both comedonal and inflammatory acne.
Adapalene 0.1% is now available over the counter in the U.S., Canada, Australia, and New Zealand. That’s a big deal. You don’t need a prescription anymore. It’s gentler than older retinoids like tretinoin, so it’s easier to start with.
Use it at night. It can cause peeling and redness at first, especially if you’re new to retinoids. But after 4 to 8 weeks, most people see smoother skin and fewer breakouts. It’s not an antibiotic, so it doesn’t fight bacteria directly-but it prevents the clogs that lead to them.
Many dermatologists now recommend starting with adapalene, then adding benzoyl peroxide if needed. Some even use it with clindamycin for a triple approach.
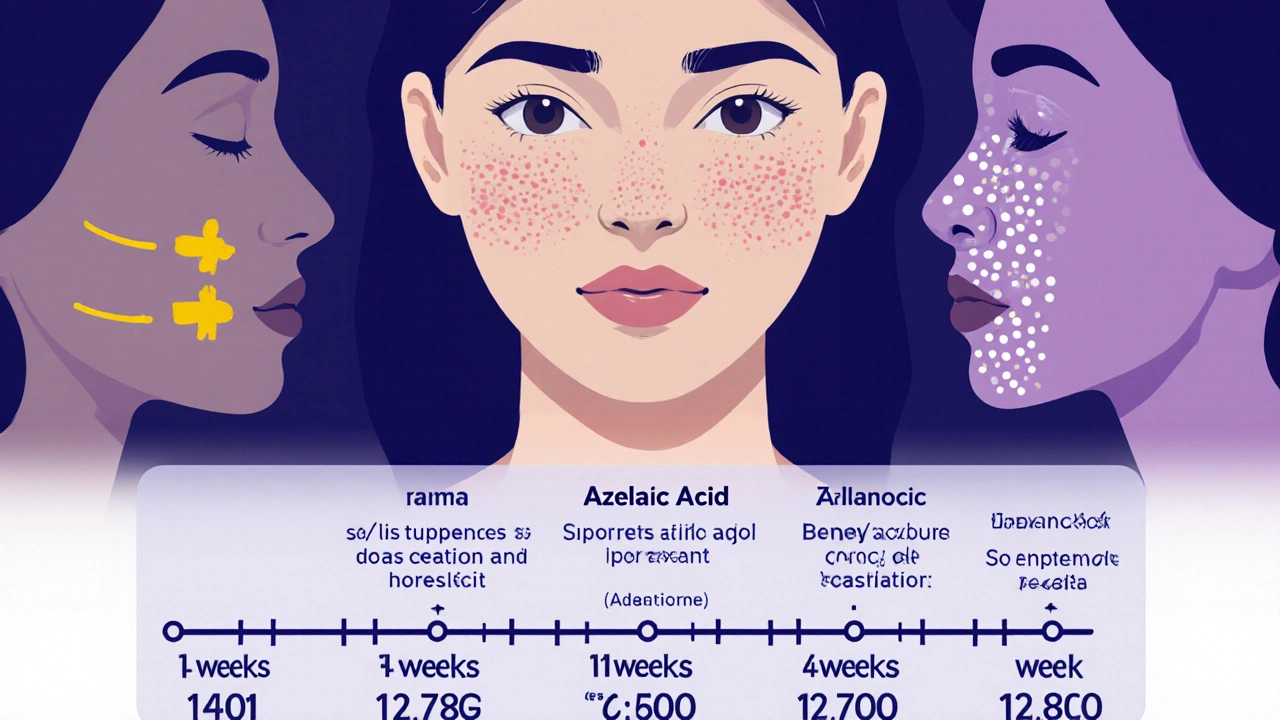
Alternative #3: Azelaic Acid (Finacea, Skinoren)
Azelaic acid is less known but just as powerful. It’s naturally found in grains like barley and wheat. In skincare, it’s used at 15%-20% concentration. It kills acne bacteria, reduces redness, and even fades post-acne marks.
It’s especially good for people with sensitive skin or rosacea. It doesn’t cause the same burning or peeling as retinoids or benzoyl peroxide. You can use it twice a day. It’s also safe during pregnancy, which makes it a top pick for expectant mothers.
Downside? It takes longer to work. You might need 8 to 12 weeks before you see real changes. But if you’ve tried everything else and your skin is still reacting badly, azelaic acid is worth a shot.
Alternative #4: Oral Antibiotics (Doxycycline, Minocycline)
If your acne is widespread, deep, or painful, topical treatments alone might not cut it. That’s where oral antibiotics come in. Doxycycline and minocycline are the most common. They work systemically-meaning they go through your bloodstream to hit acne bacteria everywhere.
They’re usually prescribed for 3 to 6 months, never longer. Long-term use increases the risk of antibiotic resistance and gut issues. That’s why they’re not a long-term solution. They’re a bridge-used to calm things down so you can switch to maintenance treatments like retinoids or benzoyl peroxide.
They’re not for mild acne. If you only have a few pimples, skip the pills. But if you’ve got 20+ inflamed breakouts across your face and chest, an oral antibiotic might be the fastest way to get relief.
Alternative #5: Spironolactone (for Hormonal Acne)
If you’re a woman and your breakouts flare up around your period, along your jawline, or on your chin-you likely have hormonal acne. Topical treatments won’t fix the root cause. That’s where spironolactone comes in.
This is a blood pressure medication that also blocks androgen hormones, which trigger excess oil and clogged pores. It’s not FDA-approved for acne, but it’s widely used off-label and backed by strong clinical data. Studies show up to 85% of women with hormonal acne see improvement.
It takes 2 to 3 months to work. Side effects include breast tenderness, fatigue, and more frequent urination. It’s not safe during pregnancy. But if you’ve tried everything else and your acne keeps coming back in the same spots, this could be the missing piece.
Comparison Table: Cleocin Gel vs Top Alternatives
| Treatment | How It Works | Best For | Time to See Results | Resistance Risk | Side Effects |
|---|---|---|---|---|---|
| Cleocin Gel (Clindamycin) | Kills acne bacteria, reduces inflammation | Inflammatory pimples, red bumps | 4-6 weeks | High (if used alone) | Dryness, irritation, rare diarrhea |
| Benzoyl Peroxide | Kills bacteria, unclogs pores | All acne types, prevention | 2-4 weeks | None | Dryness, bleaching, stinging |
| Adapalene (Differin) | Unclogs pores, reduces inflammation | Blackheads, whiteheads, mild acne | 6-12 weeks | None | Peeling, redness, initial flare-up |
| Azelaic Acid | Kills bacteria, fades marks, reduces redness | Sensitive skin, post-acne marks, rosacea | 8-12 weeks | Low | Mild stinging, rarely itching |
| Doxycycline (Oral) | Systemic antibacterial | Severe, widespread acne | 4-8 weeks | Medium (with long-term use) | Stomach upset, sun sensitivity |
| Spironolactone | Blocks hormones that cause oil | Hormonal acne (jawline, chin) | 2-3 months | N/A | Fatigue, frequent urination, menstrual changes |
Who Should Stick With Cleocin Gel?
You might still be fine using Cleocin Gel-if you’re using it the right way. Here’s when it makes sense:
- You’re using it with benzoyl peroxide (in a combo product)
- Your acne is mostly red, inflamed bumps-not blackheads
- You’ve tried retinoids and they irritated your skin too much
- You’re pregnant or breastfeeding and need a safe option
If none of those apply, it’s time to reconsider. Cleocin Gel isn’t bad-it’s just not enough on its own.
Who Should Try Something Else?
Switch if:
- You’ve been on it for 8+ weeks and see no improvement
- Your acne keeps coming back after stopping
- You’ve noticed more whiteheads or clogged pores
- Your skin feels dry, tight, or irritated all the time
- You’re using it alone, without benzoyl peroxide
In these cases, adapalene or benzoyl peroxide are safer, more sustainable choices. Azelaic acid is ideal if your skin is sensitive. And if your breakouts follow your cycle, spironolactone could be life-changing.
What to Do Next
Don’t stop your current treatment cold turkey. That can cause a flare-up. Instead:
- Take a photo of your current acne. This helps you track changes.
- Ask your dermatologist if you can add benzoyl peroxide to your routine.
- If you’re not already using it, try a low-dose adapalene gel at night.
- If your skin reacts badly, switch to azelaic acid.
- If your acne is deep or hormonal, ask about oral antibiotics or spironolactone.
Most people don’t need to try every option. Usually, one or two changes are enough to get results. The key is consistency. Acne treatments take time. But when you find the right combo, your skin will thank you.
Can I use Cleocin Gel every day?
Yes, Cleocin Gel is designed for daily use-usually once a day, often at night. But using it alone increases the risk of antibiotic resistance. Always pair it with benzoyl peroxide unless your doctor advises otherwise.
How long does it take for Cleocin Gel to work?
Most people start seeing fewer red pimples in 4 to 6 weeks. Full results can take up to 12 weeks. If you don’t see improvement after 8 weeks, talk to your doctor about switching or adding another treatment.
Is Cleocin Gel better than Differin?
It depends on your acne type. Cleocin Gel works best for inflamed, red pimples. Differin (adapalene) is better for blackheads, whiteheads, and preventing clogs. Many dermatologists recommend using both together for the best results.
Can I use Cleocin Gel while pregnant?
Yes, topical clindamycin is considered safe during pregnancy. It’s one of the few acne treatments approved for use while expecting. Avoid oral antibiotics and retinoids during pregnancy unless specifically directed by your doctor.
Why does my skin get worse before it gets better?
This is common with retinoids like Differin, and sometimes with benzoyl peroxide. Your skin is adjusting. It usually lasts 2 to 4 weeks. If you’re using Cleocin Gel alone, worsening acne may mean it’s not working anymore-or bacteria have become resistant. Talk to your doctor if your acne gets worse after 2 weeks.
What’s the best over-the-counter alternative to Cleocin Gel?
Adapalene 0.1% gel (Differin) is the best OTC alternative. It’s proven effective for all types of acne, doesn’t cause resistance, and is available without a prescription in New Zealand and many other countries. Benzoyl peroxide 2.5% is also a strong OTC option.






14 Comments