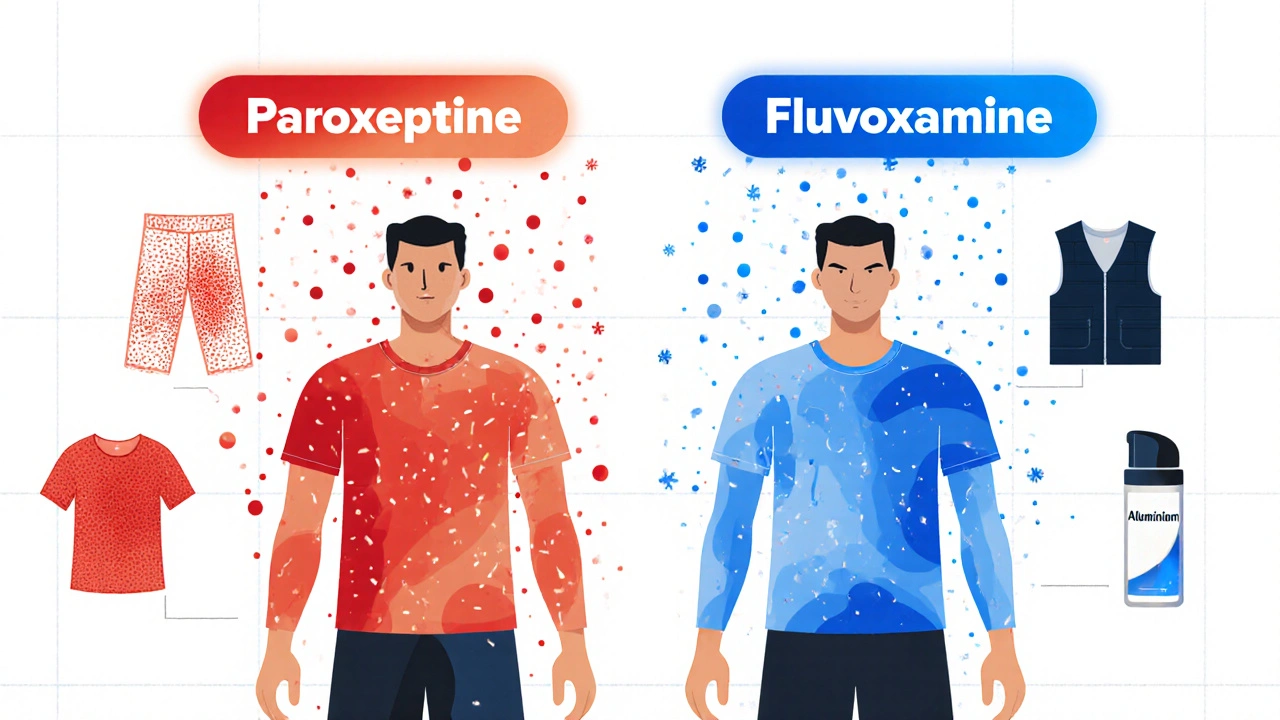
More than 1 in 10 people taking antidepressants experience sweating so heavy it soaks through clothes, ruins sleep, and makes social situations unbearable. This isn’t just discomfort-it’s a leading reason people quit their meds, even when the depression is improving. Known as antidepressant-induced excessive sweating (ADIES), this side effect affects 7% to 22% of users, with some drugs like paroxetine and sertraline triggering it in nearly 1 in 5 patients. And unlike nausea or drowsiness, this symptom rarely fades with time. If you’re drenched by noon, waking up soaked at 3 a.m., or avoiding meetings because your armpits are visible through your shirt, you’re not alone-and you don’t have to live with it.
Why Do Antidepressants Make You Sweat So Much?
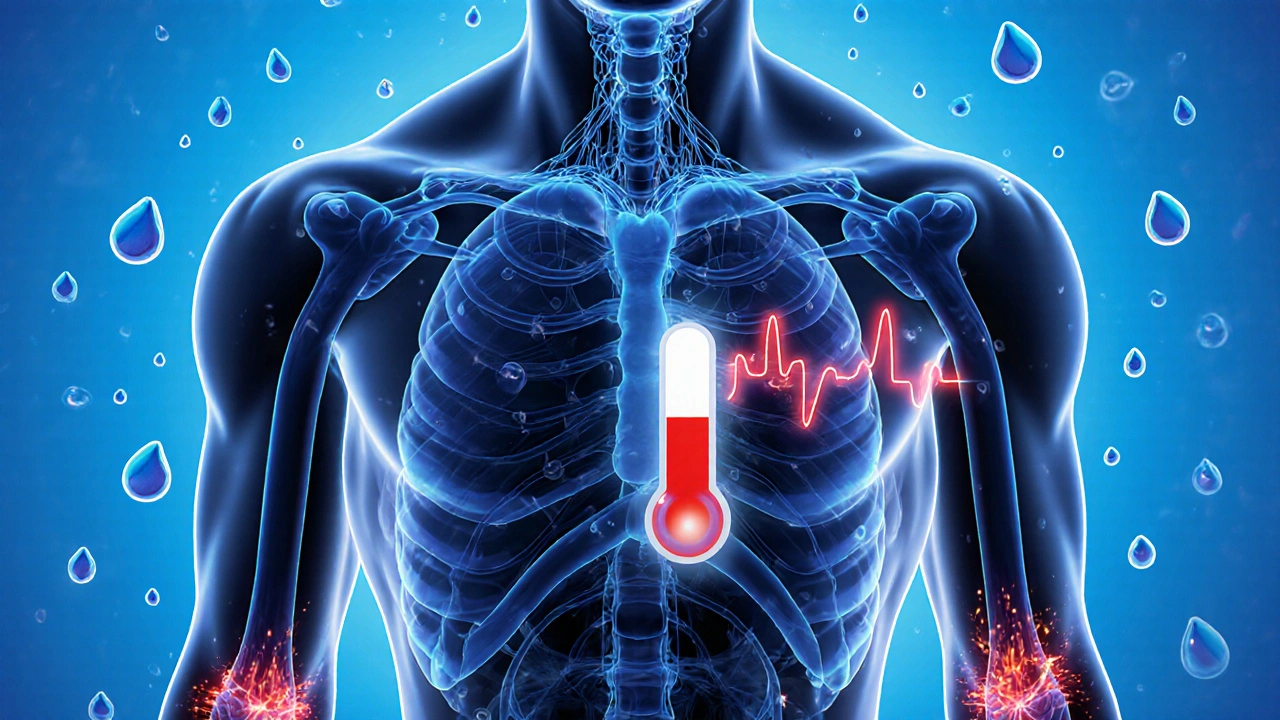
It’s not your body overheating. It’s your brain’s thermostat getting mixed signals. Antidepressants, especially SSRIs and SNRIs, boost serotonin levels. That’s good for mood-but serotonin also talks directly to the hypothalamus, the part of your brain that controls body temperature. Too much serotonin? Your brain thinks you’re burning up, even when you’re sitting in a cool room. The result? Sweat glands go into overdrive.
This isn’t just about SSRIs. SNRIs like venlafaxine, tricyclics like amitriptyline, and even bupropion can trigger it. The mechanism is the same: disrupted thermoregulation. What’s different is how often it happens. Paroxetine? Up to 19% of users report heavy sweating. Fluoxetine? Closer to 7%. Sertraline? Around 10%. And even small changes in the chemical structure matter-switching from escitalopram to citalopram (same dose, slightly different molecule) has been shown to stop sweating completely in some cases.
Which Antidepressants Are Least Likely to Cause Sweating?
If you’re struggling with sweating, your medication choice matters more than you think. Not all antidepressants are created equal when it comes to this side effect. Here’s what the data shows:
| Medication | Sweating Incidence | Notes |
|---|---|---|
| Paroxetine (Paxil) | 19% | Highest risk; often causes severe sweating |
| Sertraline (Zoloft) | 10% | Common trigger; affects many users |
| Escitalopram (Lexapro) | 14% | Higher than citalopram due to stereochemistry |
| Citalopram (Celexa) | 7% | Lower risk than escitalopram; good switch option |
| Fluoxetine (Prozac) | 7% | Lower incidence; longer half-life may help |
| Fluvoxamine (Luvox) | 3% | Lowest risk among SSRIs |
| Venlafaxine (Effexor) | 12% | SNRI; higher risk than SSRIs in some studies |
| Bupropion (Wellbutrin) | 8% | Less sexual side effects but similar sweating rates |
| Trazodone | 4% | Often used off-label; low sweating risk |
| Vortioxetine (Trintellix) | 5% | Newer agent; significantly lower risk |
Bottom line: If you’re sweating heavily, your current drug might be the problem. Fluvoxamine, citalopram, trazodone, and vortioxetine are your safest bets. Switching isn’t always easy-but it’s often the most effective fix.
Non-Drug Cooling Strategies That Actually Work
Before you change your medication, try these practical, no-prescription-needed fixes. They won’t cure the root cause-but they can make life bearable while you figure out your next step.
- Moisture-wicking clothing: Skip cotton. It holds sweat and takes forever to dry. Look for athletic fabrics like polyester blends or merino wool. Brands like Under Armour, Icebreaker, and Smartwool make shirts and undershirts designed to pull sweat away from skin.
- Cooling vests: A 2022 pilot study found that wearable cooling vests reduced sweating symptoms by 60% in antidepressant users. These aren’t fancy-they’re simple vests with gel packs or phase-change materials that stay cool for hours. You can wear them under a shirt and hardly notice.
- Antiperspirants with aluminum chloride: Regular deodorant won’t cut it. Use a clinical-strength antiperspirant with 15-20% aluminum chloride. Apply it at night to dry skin. It clogs sweat glands temporarily. Works best on underarms, but can be used on palms or soles with caution.
- Keep your environment cool: Use a fan at night. Set your thermostat to 66-68°F. Sleep with a damp washcloth on your neck. These small changes can cut night sweats dramatically.
- Hydrate smartly: Drink water, but avoid caffeine and alcohol. Both raise body temperature and can make sweating worse.
One user on Reddit reported going from three outfit changes a day to just one after switching to moisture-wicking undershirts and using aluminum chloride antiperspirant nightly. It didn’t stop the sweating-but it stopped the shame.
Medications That Can Help Reduce Sweating
If lifestyle changes aren’t enough, your doctor can prescribe something to directly block the sweating. These aren’t first-line, but they’re proven for ADIES.
- Glycopyrrolate (1-2 mg daily): An anticholinergic that blocks sweat gland signals. Starts working in days. Side effects: dry mouth, constipation, blurred vision. Most users tolerate it well at low doses.
- Benztropine (0.5-1 mg daily): Another anticholinergic, often used for Parkinson’s. Shown to reduce sweating by 75% in case studies. Less drying than glycopyrrolate for some.
- Terazosin (1-5 mg at night): A blood pressure med that also blocks alpha-receptors involved in sweating. Works especially well for night sweats. Can cause dizziness when standing-take it at bedtime.
Important: These aren’t magic pills. They’re tools to buy time while you and your doctor decide whether to switch antidepressants. Don’t stop your antidepressant without medical supervision. But adding one of these can make the difference between quitting your meds and sticking with them.
When to Consider Switching Antidepressants
Switching isn’t failure-it’s strategy. Many people assume they have to stick with the first drug that helped their mood. But if sweating is wrecking your life, a switch could be the best decision you make.
Good candidates for switching:
- You’re on paroxetine, sertraline, or escitalopram and sweating daily
- You’ve tried cooling strategies and antiperspirants for 4-6 weeks with no relief
- You’re not improving on your current dose
Best switches based on research:
- Escitalopram → Citalopram: Same dose, different molecule. One case report showed complete resolution of sweating.
- Sertraline or paroxetine → Fluvoxamine: Lowest sweating risk among SSRIs.
- Any SSRI/SNRI → Trazodone or Vortioxetine: Low sweating risk, good mood benefits.
Don’t switch cold turkey. Work with your prescriber to taper slowly and cross-taper. Some people need to go through a few meds before finding the right fit. But many report life-changing results after just one switch.

Don’t Mistake Sweating for Serotonin Syndrome
Heavy sweating alone is ADIES. But if you’re sweating and you have:
- Shaking or tremors
- Rapid heartbeat
- High fever (over 101°F)
- Muscle rigidity
- Confusion or hallucinations
-this could be serotonin syndrome. It’s rare but dangerous. Stop your medication and go to the ER immediately. ADIES is uncomfortable. Serotonin syndrome can kill you.
What’s Next? The Future of Managing This Side Effect
Things are getting better. New antidepressants like LS-2-1123, currently in Phase II trials, show only 3.2% sweating rates-far lower than escitalopram’s 14.7%. Transdermal patches (like selegiline) cut sweating by 60% compared to pills. And by 2027, doctors may test your genes to predict if you’re likely to sweat from certain meds.
Right now, you have options. You don’t have to suffer in silence. You don’t have to quit your antidepressant. You just need the right strategy.
Can antidepressant sweating go away on its own?
In most cases, no. Unlike nausea or dizziness, which often fade after a few weeks, antidepressant-induced sweating rarely improves with time. Studies show symptoms persist beyond six months for most patients. Waiting it out isn’t a reliable strategy-active management is needed.
Is sweating a sign my antidepressant isn’t working?
Not necessarily. Sweating is a side effect, not a sign of treatment failure. Many people experience heavy sweating while their depression improves. The issue isn’t whether the drug is working-it’s whether the side effect is unbearable. That’s a quality-of-life decision, not a clinical one.
Can I use over-the-counter antiperspirants for antidepressant sweating?
Regular deodorants won’t help. You need clinical-strength antiperspirants with 15-20% aluminum chloride. Brands like Certain Dri, Drysol, or Odaban are available OTC. Apply at night to dry skin. It’s not perfect, but it reduces sweat volume by 50-70% for many users.
How long does it take to see results after switching antidepressants?
It varies. Some people notice less sweating within a week of switching. Others take 2-4 weeks as their body adjusts. If you switch from a high-risk drug like paroxetine to a low-risk one like fluvoxamine or citalopram, you should see improvement within 10-14 days. Don’t give up before then.
Are there any natural remedies that help with antidepressant sweating?
No natural remedy has been proven to stop antidepressant-induced sweating. Herbal supplements like sage or witch hazel may offer mild relief for general hyperhidrosis, but they don’t block the brain-driven mechanism behind ADIES. Stick with science-backed strategies: cooling clothing, antiperspirants, or medical options like glycopyrrolate. Don’t risk interactions or false hope with unproven supplements.





9 Comments